What Is Stage 4 Cancer?
What is stage 4 cancer? It means the cancer has spread from its original site to distant parts of the body. This spread, known as metastasis, defines cancer as being “stage 4” or “metastatic.” Cancer cells break away from the primary tumour. They travel through the bloodstream or lymphatic system. Then they form new tumours in other organs or tissues. This represents the most advanced stage of cancer.
What does stage 4 cancer mean for your treatment journey? A stage 4 cancer diagnosis is serious. But understanding your options and having the right support makes a difference. It can improve both your quality of life and survival time.
Contact Me for Expert Guidance
Is Stage 4 Cancer Terminal?
Is stage 4 cancer terminal? This is one of the most common questions people search online. It reflects the fear and uncertainty that comes with such a diagnosis. Stage 4 cancer is serious. In many cases it may not be curable in the traditional sense. But modern treatments can often extend life significantly. They can also maintain good quality of life.
Don’t rely on internet searches for answers to profound questions. I strongly encourage you to speak with your healthcare team. As a specialist with over 23 years of experience, I can tell you this. Doctors and specialist nurses have heard these questions many times before. They should be ready to provide you with personalised information.
Can You Survive Stage 4 Cancer?
Can you survive stage 4 cancer? This is a complex question that depends on many factors. These include the type of cancer, your overall health, and available treatment options. Stage 4 cancer means the cancer has spread to distant parts of the body. Survival rates vary widely between different cancers.
For most solid tumours that have spread, curative treatment may not be possible. But this doesn’t mean effective treatments aren’t available. We can extend your life and maintain its quality with the right approach.
Stage 4 Cancer Life Expectancy With Treatment
Stage 4 cancer life expectancy with treatment has improved significantly in recent years. Modern approaches often extend survival beyond historical expectations. This is particularly true for certain types. These include stage 4 lung cancer, stage 4 breast cancer, and stage 4 bowel cancer.
A few decades ago, stage 4 cancer survival rates were generally poor. Today, we have advanced treatments. These include immunotherapy, targeted therapy, and precision radiotherapy. Many patients now live longer and better lives after a stage 4 diagnosis.
Statistics reflect populations, not individuals. Your personal journey may differ from the average. I’ve seen many patients defy the odds with the right treatment approach.
Stage 4 Cancer Treatment Options
When facing stage 4 cancer, comprehensive treatment typically involves multiple approaches:
Systemic Therapies
The backbone of stage 4 cancer treatment is typically systemic therapy. These treatments work throughout your entire body. They target cancer cells wherever they may be:
- Immunotherapy – Enhances your immune system’s ability to recognise and attack cancer cells
- Targeted Therapy – Precision medicines that target specific genetic changes in cancer cells
- Chemotherapy – Traditional treatments that kill rapidly dividing cells
These systemic treatments form the foundation of care for many cancers. This includes stage 4 lung cancer, stage 4 breast cancer, stage 4 bowel cancer, and stage 4 prostate cancer.
Local Treatments for Stage 4 Cancer
Local therapies can be crucial alongside systemic treatments. They control symptoms and sometimes eliminate visible metastases:
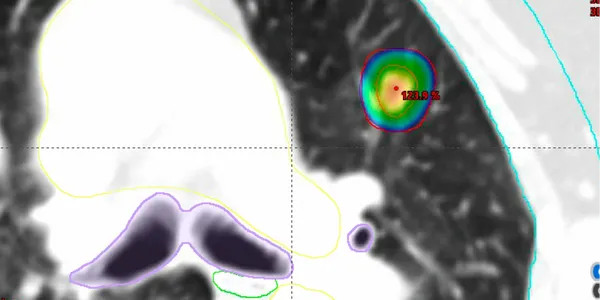
- Stereotactic Radiotherapy – Highly precise, high-dose radiation that can eradicate metastatic sites
- Surgery – In select cases, surgical removal of metastases may help
- Conventional Radiotherapy – Effectively manages symptoms like pain from bone metastases

Can Immunotherapy Cure Stage 4 Cancer?
Can immunotherapy cure stage 4 cancer? Complete cures remain relatively rare. Yet immunotherapy has revolutionised the treatment landscape for many cancers. This includes stage 4 lung cancer, stage 4 melanoma skin cancer, and others. Some patients experience remarkable responses. Some achieve long-term disease control that may extend for years or decades.
Combined with other treatments like stereotactic radiotherapy, immunotherapy can be even more effective. This potentially improves stage 4 cancer survival rates.
Setting Priorities for Stage 4 Cancer Care
If you have stage 4 cancer, establishing your priorities for treatment is essential. Consider these principles:
- Quality of Life – Don’t accept treatments that make you feel worse than your cancer does
- Access to Advanced Options – Ensure you can access the best treatments for your specific cancer type
- Family Involvement – Cancer affects not just you but those who love you; include them in your journey
- Open Communication – Discuss your wishes, fears, and goals openly with your healthcare team
When Should You Talk About End-of-Life Care?
As a society, we often avoid discussing death. But in my experience, talking about end-of-life wishes early can enhance your quality of life. Have these conversations while you’re still feeling relatively well. This allows you to express your preferences. You can put your mind at rest. Then you can focus on living well.
Stage 4 cancer prognosis varies widely by cancer type. Some, like stage 4 pancreatic cancer, have more challenging outlooks. Others, such as certain forms of stage 4 prostate cancer or stage 4 breast cancer, may have more favourable outcomes.
Having these conversations isn’t “giving up.” It’s taking control of your care. It ensures your wishes are respected.
Finding the Right Specialist for Stage 4 Cancer
When faced with stage 4 cancer, having the right specialist makes a difference. You need a doctor who:
- Can recommend appropriate systemic treatments
- Has access to advanced local treatments like stereotactic radiotherapy
- Knows when to revisit treatment options if you respond well initially
- Communicates clearly about what success looks like
- Respects your priorities and quality of life concerns
I have extensive experience treating advanced cancers. This includes stage 4 lung cancer, stage 4 skin cancer, and stage 4 melanoma. I understand the importance of personalised care. This addresses both extending life and maintaining its quality.
Stage 4 Cancer: A Team Approach
Treating stage 4 cancer is truly a team effort. This isn’t just among medical professionals. It includes your family as well. While it’s your body experiencing the cancer, the impact extends to those who care about you.
Include your loved ones in your treatment decisions. Allow them to support you. This makes a tremendous difference in your journey. They can help advocate for you. They provide emotional support. They assist with practical matters. They ensure your wishes are respected.
Beyond Statistics: Living with Stage 4 Cancer
Stage 4 cancer survival rates and life expectancy reflect populations, not individuals. I’ve seen patients with advanced cancers significantly outlive initial prognoses. This includes those with stage 4 lung cancer and stage 4 bowel cancer.
Modern treatments continue to improve outcomes for stage 4 cancer. What had a dire prognosis just a few years ago might now have multiple treatment options.
Taking the Next Step
Have you or a loved one been diagnosed with stage 4 cancer? Are you searching for answers to questions? Examples include “how long can you live with stage 4 cancer” or “is stage 4 cancer curable.” I encourage you to seek expert guidance. Don’t rely solely on internet searches.
As a specialist in treating advanced cancers, I can provide personalised information. I can explain treatment options that might be available to you. I can help you navigate this challenging journey with clarity and support.
Together, we can develop a treatment approach with dual focus. We’ll aim to extend your life. We’ll also give life to the time you have. We’ll address your symptoms. We’ll optimise your quality of life. We’ll help you achieve what matters most to you.
Expert-Led Training on Skin Cancer Radiotherapy Options
Are you a healthcare professional looking to expand your knowledge of basal cell skin cancer treatment and squamous cell skin cancer treatment options? This comprehensive educational resource features Dr. James Wilson, a leading oncology skin cancer specialist, sharing his expertise on non-surgical approaches to skin cancer management.
Why Consider Radiotherapy for Skin Cancer Treatment?
Radiotherapy offers an effective alternative to surgery for many patients with non-melanoma skin cancers. This educational video provides detailed insights into:
- Characterising risk in basal cell carcinoma and squamous cell carcinoma
- When to recommend skin cancer radiotherapy over surgical options
- Different types of radiotherapy techniques and their applications
- Treatment scheduling and patient care protocols
- Managing side effects and follow-up care
Find the Right Skin Cancer Treatment for Your Patients
For GPs, dermatologists, dermatological surgeons, plastic surgeons, and other healthcare professionals who encounter patients with skin cancer, understanding all available treatment modalities is essential for providing optimal care.

Key Topics Covered in This Educational Resource
Basal Cell Skin Cancer Treatment Options
Learn how to spot risk factors for basal cell carcinoma and when radiotherapy for basal cell skin cancer works best. In this part, Dr. Wilson clearly explains:
- How to group different BCC types by risk
- How to set margins for nodular vs infiltrative BCCs
- Radiotherapy methods that work well for facial BCCs
- Real patient cases showing good cosmetic results
Squamous Cell Skin Cancer Treatment Approaches
Next, learn about the newest ways to use radiotherapy for squamous cell skin cancer treatment, including:
- High-risk features that need special care
- When to use radiotherapy as first treatment vs after surgery
- How to treat patients with weak immune systems
- How to follow up with patients based on their risk level
Advanced Radiotherapy Planning and Techniques
Also, learn in-depth about:
- X-ray radiotherapy
- When and how to use electron beam therapy
- How to use 3D-printed custom bolus for tricky body areas
- New methods like Rhenium-SCT topical brachytherapy
Real Patient Cases and Treatment Results
This resource includes detailed patient cases showing:
- Before and after pictures of treatments
- How to manage side effects
- Long-term cosmetic results
- What patients say about their treatment
Who Should Watch This Educational Resource?
This training is very useful for:
- GPs who treat skin cancer patients
- Skin doctors looking for non-surgical options
- Surgeons thinking about using multiple treatment types to improve treatment results
- Cancer specialists who focus on skin cancer
- Health workers who treat older or medically complex patients
Making Treatment Decisions Based on Evidence
Also, learn how to weigh these three key factors when choosing skin cancer treatment:
- Chance of cure: Understanding success rates for different treatments
- How it will look: Comparing radiotherapy vs surgical results for different body areas
- Patient comfort: Thinking about treatment length, visits needed, and healing time
Access This Essential Educational Resource Now
Watch our video to boost your knowledge of basal cell skin cancer treatment and squamous cell skin cancer treatment options. You’ll feel more confident discussing all options with your patients and making smart suggestions based on each person’s needs.
Keep Learning About Skin Cancer Management
Stay up-to-date on skin cancer care by knowing when skin cancer radiotherapy works better than surgery, especially for:
- Patients with weak immune systems who need extra treatment
- Older patients with other health issues
- Patients taking blood thinners
- Face lesions that would need complex rebuilding
- Hard-to-treat spots (eyelids, nose, ears)
This educational resource is provided for healthcare professionals to enhance clinical knowledge and improve patient care outcomes.
Introduction to Basal Cell Carcinoma
Radiotherapy is a highly effective treatment for basal cell carcinoma (BCC), the most common type of skin cancer worldwide. It develops in the basal cells, which are found in the outer layer of your skin, the epidermis. The main cause is long-term exposure to sunlight. You may be more likely to develop this cancer if you have fair skin, have had bad sunburns, have been exposed to certain chemicals, or have a weakened immune system. It’s important to protect yourself by avoiding too much sun exposure and using proper sun protection.
These skin cancers often look like a small, shiny bump or a patch on your skin. They can be flesh-coloured, pink, or slightly darker than your surrounding skin. Unlike other skin cancers, BCC usually grows slowly and very rarely spreads to other parts of your body. However, if left untreated, it can damage nearby tissues and cause scarring.
Early diagnosis and treatment are very important. Your skin specialist (dermatologist) will usually examine your skin carefully and may take a small sample (biopsy) to confirm if it’s BCC. Finding and treating it early means simpler treatment is often possible. There are two main treatment options: radiotherapy and surgery. Understanding what BCC is and your treatment choices will help you make informed decisions about your care.
Overview of Treatment Options for BCC
If you’ve been diagnosed with basal cell carcinoma (BCC), you have several treatment options. The main ones are surgery, radiotherapy, skin creams, and light therapy. Each has its own benefits and drawbacks, and what’s right for you depends on your particular situation.
Surgery remains the most common treatment for BCC, especially when the cancer is in one spot and easy to reach. The most precise type of surgery is called Mohs surgery, which carefully removes the cancer while saving as much healthy skin as possible. This is particularly useful for cancers on the face. However, surgery might not be suitable for everyone, especially if you have certain health conditions or take particular medications.
Radiotherapy is an effective alternative, particularly if surgery isn’t suitable. It uses high-energy x-rays to target and destroy cancer cells. While it doesn’t involve cutting, it can cause some temporary skin irritation.
Skin creams containing special medicines can help with surface (superficial) BCCs, especially if you prefer a treatment without surgery. These creams are applied directly to your skin.
Light therapy uses special light-sensitive medicine and light to destroy cancer cells. This is usually only used for superficial BCCs and offers a non-surgical option with quick recovery time. Your healthcare team will consider your cancer’s size and location, as well as your overall health, to recommend the best treatment option for you.
Understanding Radiotherapy: How It Works
Radiotherapy is an important treatment option for people with basal cell carcinoma (BCC). It works by using targeted radiation to damage cancer cells, which stops them from growing and causes them to die. The treatment aims to destroy the cancer cells while causing as little harm as possible to surrounding healthy skin.
There are two main types of radiotherapy: external beam radiotherapy and radiotherapy that comes from radioactive material placed close to the skin (also called brachytherapy). External beam radiotherapy directs x-rays from outside your body towards the cancer.
Rhenium-SCT (Rhenium-188 topical therapy) offers several unique advantages for selected BCC patients. This single-visit treatment applies a radioactive paste directly to the skin cancer, with clinical studies showing:
- 97.5% response rates at 12 months
- 95% complete responses
- Superior cosmetic outcomes in 41% of cases
Your treatment will begin with a consultation where your doctor will assess your condition and overall health. You might need some scans to help plan your treatment. Once the plan is ready, you’ll have several treatment sessions, usually over a 1-2 weeks. Each session typically lasts only a few minutes, during which you’ll need to lie still while the radiotherapy machine is precisely positioned. Rhenium-SCT only requires one visit of usually around an hour or two.
Most people cope well with radiotherapy for BCC, though you might experience some side effects like skin irritation or tiredness in the weeks after treatment. It’s important to keep talking with your doctor, as they can help you manage any side effects. Radiotherapy can be particularly helpful for people who can’t have surgery, have recurring BCC, or have high-risk BCC.

(A before and after image of a BCC on the nose that was successfully treated with radiotherapy)
Surgical Treatments for BCC: An Overview
There are different types of surgery available for treating basal cell carcinoma (BCC). One of the most advanced techniques is Mohs surgery, which is a specialised procedure that removes the cancer layer by layer. During this surgery, each layer is checked under a microscope to ensure all cancer cells are removed while saving as much healthy skin as possible. This type of surgery is often recommended for BCCs on the face, neck, and ears, where appearance is particularly important.
Another common option is standard surgery, where the surgeon removes the cancer along with a small margin of healthy skin around it. This method effectively removes BCC and can be done in most areas of the body. While it might not be as precise as Mohs surgery, it’s usually quicker and simpler, and can often be done as an daycase procedure.
After surgery, you might experience some swelling, bruising, or discomfort in the treated area, but this usually improves over time. Sometimes, you might need additional surgery with a plastic or dermatological surgeon to improve the appearance of the treated area. This depends on the size and location of the original surgery.
Your doctor will help you choose the most appropriate type of surgery based on several factors, including where your BCC is located, its size, your general health, and what you prefer. It’s important to discuss these options with your healthcare team to understand which approach might work best for you.
Pros and Cons of Radiotherapy for BCC
Radiotherapy is a common treatment option for basal cell carcinoma (BCC), particularly for people who might not be suitable for surgery. One of the main advantages is that it doesn’t involve any cutting. Unlike surgery, radiotherapy can be given as an outpatient treatment, which means you remain at home with minimal disruption to your daily routine.
Another benefit of radiotherapy is that it works well for certain groups of people, especially those with larger skin cancers or those who can’t have surgery due to age or other health conditions. In these cases, radiotherapy can effectively target the cancer while protecting the surrounding healthy tissue. Many people also find they have fewer immediate side effects compared to surgery.
However, radiotherapy does have some drawbacks. While your radiotherapy is designed to minimise damage to healthy areas, you might experience side effects such as skin irritation and tiredness. In very rare cases, there’s a small risk of developing another cancer in the treated area many years later. The risk of this is small and occurs many years after treatment (risk of second cancer 3:1000 at 10 years and 5:1000 at 15 years after radiotherapy).
Also, radiotherapy treatment usually requires more hospital visits than surgery, as you’ll need several sessions over a period of 1-2 weeks. This longer treatment time can be inconvenient for some people.
Pros and Cons of Surgery for BCC
When considering treatment for basal cell carcinoma (BCC), surgery is one of the most traditional approaches. The main advantage of surgery is that it completely removes the cancer cells. Surgical procedures, such as standard excision or Mohs surgery, focus on making sure all the cancer is removed, which means there’s less chance of it coming back.
Surgery often provides immediate results, which can be reassuring for many people. You can usually see straight away that the cancer has been removed, which can reduce worry about ongoing treatment. The success rate of surgery is very good, and your doctor can check the removed tissue to confirm that all the cancer cells have been taken out.
However, surgery does have some disadvantages. One main concern is scarring. Depending on where the surgery was done and how much skin needed to be removed, you might have a visible scar. Sometimes, you might need further cosmetic procedures to improve how the scar looks. Also, like any surgery, there are risks such as infection or slow healing and swelling, particularly if you’re older or have other health conditions.
Recovery time is another thing to consider. Unlike some non-surgical treatments, you’ll need time to heal after surgery, during which you might need to limit your activities. While many people have successful outcomes with surgery, it’s important to carefully consider these pros and cons. Your healthcare team will help you decide if surgery is the right choice for you.
Factors Influencing Treatment Choice
The decision between radiotherapy and surgery for treating basal cell skin cancer (BCC) depends on many factors that are specific to you. First, the characteristics of your skin cancer play a big role. The size, depth, and location of the cancer can help determine whether surgery or radiotherapy would work better. For example, smaller cancers in easy-to-reach areas might be better suited for surgery, while larger or more complicated ones might respond better to radiotherapy. Radiotherapy is particularly good for BCCs around the eyes, nose and lips.
Age is another important factor to consider. Older people might have other health conditions that make surgery more risky, making radiotherapy a better option. Younger people might prefer surgery to avoid the longer treatment schedule of radiotherapy. Your overall health is also important; if you have a weakened immune system or other health problems, this might affect which treatment is safer for you. Your doctor will carefully consider your medical history and current health when recommending treatment.
Your personal preferences are also very important in making this decision. Some people might feel anxious about having surgery, while others might prefer the quicker results that surgery can provide. Your healthcare team will discuss all available options with you, explaining the potential benefits and drawbacks of each treatment method. By carefully considering these factors, you can make an informed choice that suits your needs, health condition, and lifestyle.
Success Rates of Surgery and Radiotherapy for BCC
When choosing between treatments for basal cell skin cancer (BCC), it’s helpful to understand how well each treatment works for different people. Medical studies give us valuable information about success rates, how often the cancer comes back, and how satisfied people are with their treatment.
Research looking at people treated with Mohs surgery, a precise type of surgical treatment for BCC, shows very good results. This method successfully removes the cancer in about 98 out of 100 cases, with the cancer coming back in fewer than 5 out of 100 cases within five years. Many people were happy with this treatment because they could see results straight away and it preserved as much healthy skin as possible.
Studies of people who had radiotherapy (often because they couldn’t have surgery) also show good results. Radiotherapy successfully controlled the cancer in about 90 out of 100 cases, with the cancer coming back in about 10 out of 100 cases over five years. People had different views about this treatment; many liked that it didn’t involve surgery, but some were concerned about the length of treatment and changes to their skin afterwards. If the cancer comes back after a long time, radiotherapy may be considered again to treat the recurrent BCC.
These findings show that both treatments can work well. Surgery might have slightly better immediate success rates, while radiotherapy remains a good option for people who can’t have, or don’t want to have, surgery. Your healthcare team will help you understand which treatment might work best for your situation.
Consultation and Making an Informed Decision
When you’re diagnosed with basal cell skin cancer, you’ll need to consider different treatment options, mainly radiotherapy and surgery. Having thorough discussions with your healthcare team is essential for making the right decision about your treatment. These discussions should start soon after diagnosis to give you enough time to consider all your options.
To get the most from these discussions, it helps to prepare. Make a list of any symptoms you’ve noticed, your medical history, and any previous treatments you’ve had. This information will help your healthcare team suggest the most suitable treatment for you. It’s useful to ask about specific aspects of your skin cancer, such as its type, size, and location, as these factors can influence whether radiotherapy or surgery would be better.
You should also ask about the benefits and risks of each treatment option. For example, surgery might remove the cancer more quickly, while radiotherapy might be easier if you have other health conditions. Important questions to ask include: How likely is the cancer to come back with each treatment? What side effects might I get? How will treatment affect my daily life? These questions will help you understand what to expect from each treatment option.
You might also want to get a second opinion to help you feel more confident about your decision. It’s important to weigh up the advantages and disadvantages of each approach, considering both your physical health and personal preferences. Having open and informative conversations with your healthcare team will help you make decisions that are right for you.
Frequently Asked Questions about treatment for BCC
Treatment Selection
Q: What determines the choice between surgery and radiotherapy for BCC?
A: Key factors include age, BCC location, size and type, general health, and personal preferences. The pros and cons of both approaches should be discussed with you before you make a final treatment decision
Q: How effective is radiotherapy for BCC?
A: Cure rates are comparable to surgery in appropriate cases, with excellent outcomes for both primary and recurrent BCCs. Ask your doctor if there are any differences in cure rates in your particular situation
Treatment Process
Q: How many treatments are needed when treating a BCC?
A: Conventional radiotherapy typically requires 5-10 daily treatments over 1-2 weeks, though there are other treatment schedules depending upon your unique situarion. Rhenium-SCT requires just one visit.
Q: What are the side effects of radiotherapy for BCC?
A: Early effects include skin irritation and mild fatigue. Late effects may include slight skin colour or texture changes. Effects are usually mild and well-tolerated. There are other less common side effects that will be discussed with you in detail. The side effects very much depend on which part of your body is being treated.
Aftercare
Q: How do I care for my skin during radiotherapy for basal cell carcinoma?
A: Key recommendations include:
- Gentle cleaning with warm water
- Avoiding soaps in the treatment area
- Using recommended moisturisers or other creams provided to you by your oncologist
- Sun protection
Q: What follow-up care is needed?
A: Regular monitoring appointments check treatment response and provide ongoing care advice.
Your medical team
Treatment is delivered by consultant clinical oncologists specialising in skin cancers, working closely with dermatologists and plastic surgeons to ensure optimal care pathways and so you can be sure that all treatment options have been considered with the aim of giving you the best results. All practices follow current evidence and guidelines from the British Association of Dermatologists and the Royal College of Radiologists.
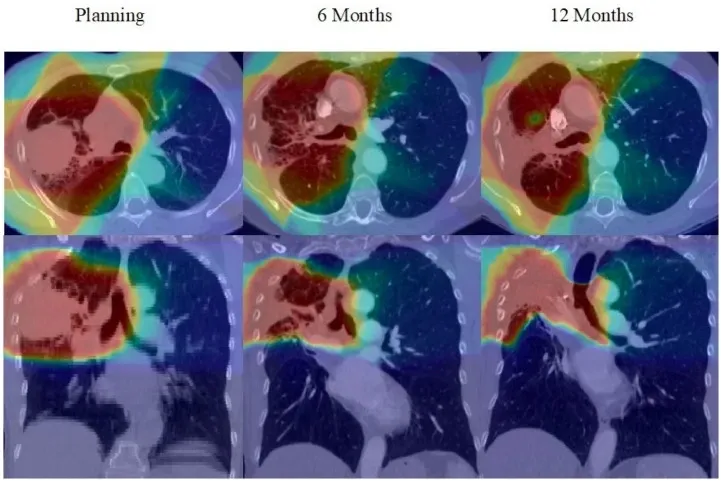
Radiotherapy is a potentially curative treatment for lung cancer. However, like all medical treatments, it comes with potential side effects, some of which may persist long after the therapy has concluded. As the effectiveness of radiotherapy for lung cancer increases, and drug treatments improve the likelihood of long-term survival for patients with lung cancer, the need to minimise side effects side effects that occur after treatment become even more important. This post explores the long-term side effects of radiotherapy for lung cancer, offering insights into management strategies and the latest advancements in treatment techniques that I offer to minimise these effects and maintain your quality of life.
What are Long-Term Side Effects?
Long-term side effects of radiotherapy are those that either continue for months after treatment or develop years later. They can vary widely among patients depending on the specific area treated, the radiation dose, and the individual’s overall health. Common long-term side effects for lung cancer patients may include:
– Lung Changes: Fibrosis (scarring of the lung tissue) is a common issue and can lead to a persistent cough or shortness of breath.
– Cardiac Effects: In some cases, radiation can affect heart health, especially if the heart was within the radiation field. This is particularly true for people who have pre-existing heart problems or risk factors.
– Oesophageal Changes: Difficulty swallowing, known as dysphagia, can occur if the oesophagus was exposed to radiation.
– Secondary Cancers: A very small increased risk of developing a second cancer in the areas treated with radiation exists. As this risk is many years after treatment, it is only now that that chance of cure is improving that this is increasing in importance. The risk is very low (3 in 1000 at 10 years, 5 in 1000 at 15 years after treatment).
It’s important to remember that not everyone experiences side effects. The benefits of eradicating cancer far outweigh the potential risks.
Management of Long-Term Effects
Managing long-term side effects involves regular monitoring and early intervention. Here are some ways to handle these persistent effects:
Pulmonary Rehabilitation
Pulmonary rehabilitation programs can help improve lung function after radiotherapy. These programs typically include exercise training, education, and support, aimed at enhancing quality of life.
Cardiac Care
For patients with potential heart issues post-radiotherapy, regular cardiovascular check-ups and monitoring might be recommended. This may include echocardiograms, ECGs and stress tests to monitor heart health and function.
Nutritional Support or oesophageal intervention
Patients experiencing oesophageal changes may benefit from dietary adjustments. If needed, a dietitian can recommend meals that are more comfortable to swallow, ensuring that nutrition does not suffer. Very rarely, we may need to perform an endoscopy to relieve any narrowing of the oesophagus to restore a normal swallow.
Prevention of long-term side effects is better than cure!
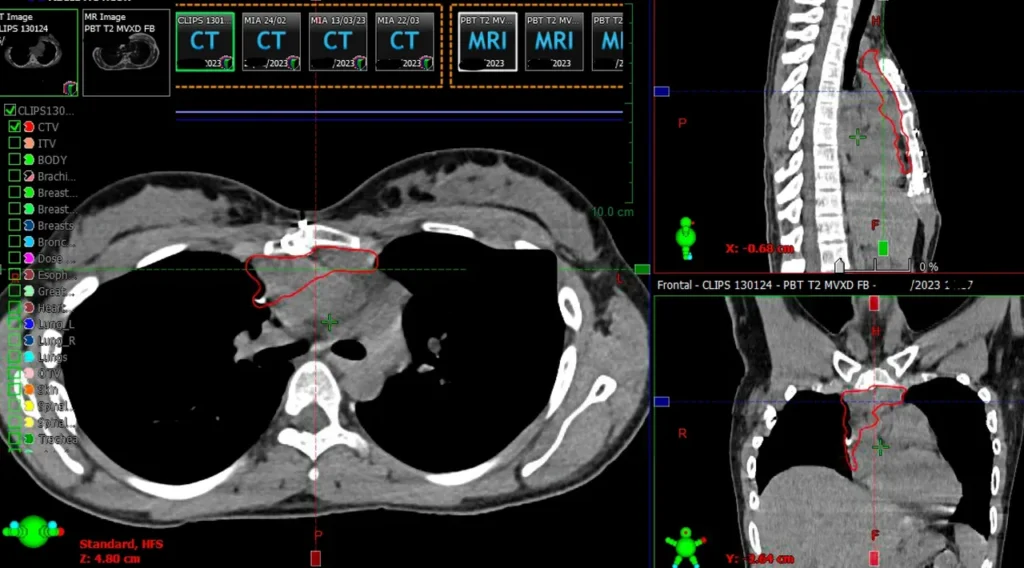
Advancements in radiotherapy techniques have dramatically improved the precision with which radiation is delivered, significantly reducing the risk of long-term side effects. At all my clinics, I utilise the latest technology and treatment protocols to ensure the highest standards of care:
Intensity-Modulated Radiotherapy (IMRT) or Volumetric Modulated Arc Therapy (VMAT)
IMRT and VMAT allow for the radiation dose to be shaped precisely around the tumour, minimising exposure to healthy tissues and reducing the risk of side effects.
Image-Guided Radiotherapy (IGRT)
IGRT helps to significantly reduce the risk of long-term side effects associated with traditional radiotherapy methods. IGRT involves frequent imaging during treatment, ensuring that radiation is accurately targeted, which is crucial for tumours that move, like those in the lung. This greatly enhances the precision and effectiveness of radiotherapy, but also ensures important, critical structures are spared from high doses of radiation.
Advanced motion management techniques
These techniques are designed to precisely target tumours while protecting healthy tissues, even as patients breathe and their internal organs naturally move. I personalise the use of these techniques to each individual patient with the aim of reducing the amount of normal tissue that receives any radiation dose and therefore reduce side effects.
– Breath-Hold Techniques
Breath-hold technologies, such as Active Breathing Control (ABC), allow doctors to deliver radiation while the lungs are in a consistent position. By instructing the patient to hold their breath at a specific point in their breathing cycle, the movement of the lung and heart is minimised. This stability enables more accurate targeting of the tumour, significantly reducing radiation exposure to healthy tissues and thus lowering the risk of heart and lung damage.
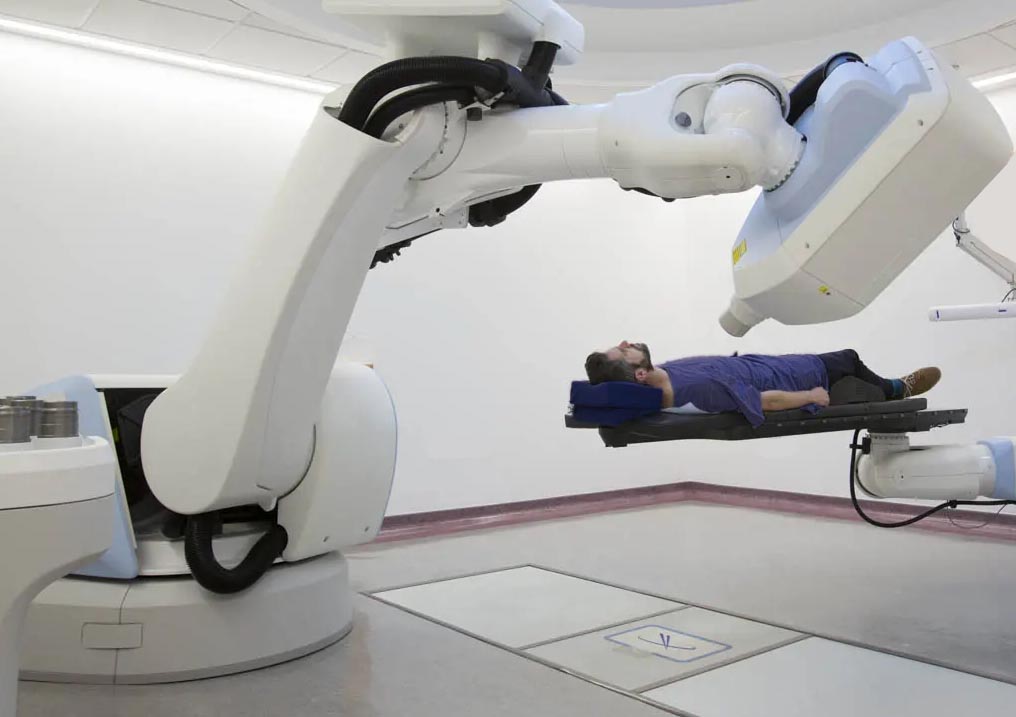
– CyberKnife Tumour Tracking
The CyberKnife system represents a revolutionary approach in radiotherapy. It features real-time tumour tracking technology, which tracks the tumour’s position during each breath and adjusts the radiation beam accordingly. This dynamic synchronisation means that even tumours that move with each breath can be targeted with extreme precision, sparing surrounding healthy tissues from unnecessary radiation and reducing side effects.
– Abdominal Compression
Abdominal compression is another effective technique used to reduce the movement of tumours in the chest and abdomen during radiation treatment. By gently compressing the abdomen, this method restricts the range of tumour motion due to breathing, which enhances the accuracy of radiation delivery. This not only improves the effectiveness of the treatment but also minimises the exposure of healthy organs to radiation.
These advanced motion management techniques represent a significant step forward in the treatment of lung cancer. By improving the precision of radiation delivery, they reduce the risk of damaging critical organs and tissues, thereby offering patients a better quality of life both during and after treatment.
Proton Therapy (PBT) for lung cancer
Proton beam therapy is a cutting-edge form of radiotherapy that is gaining traction in the treatment of lung cancer due to its precision and potential to reduce long-term side effects. Unlike traditional radiotherapy that uses X-rays, proton therapy uses protons — positively charged particles — which have a unique advantage. They can be programmed to deliver their energy directly to the tumour site with remarkable precision, minimising exposure to surrounding healthy tissues.
Proton beam therapy offers a type of radiation that stops at the tumour, significantly reducing the dose delivered to the surrounding normal tissues and thereby lowering the risk of long-term damages. In selected patients, those most at risk of long-term or serious side effects, I can treat patients with proton beam therapy at Proton International London (https://www.protonintlondon.com/consultants/dr-james-wilson/)
The ability of proton beam therapy to precisely target tumours means that higher doses of radiation can be used to kill cancer cells while sparing healthy tissues and organs. This can lower the incidence of side effects that patients might experience both during and after treatment.
Another potential benefit of proton therapy is its potential to reduce the likelihood of secondary cancers. Secondary cancers are a serious concern for long-term survivors of lung cancer, often triggered by exposure of healthy tissues to radiation. By limiting this exposure, proton therapy helps to minimise the risk of developing new cancers later on.
For patients undergoing lung cancer treatment, proton beam therapy offers a hopeful path with fewer long-term health concerns. This technique embodies the advancements in medical technology aimed at not just treating cancer more effectively, but also enhancing the quality of life for survivors by minimising adverse effects.
Coping with Long-Term Side Effects
Coping with long-term side effects can be challenging, but with the right strategies and support, many patients manage their symptoms effectively. All the patients that I treat are given access to all the necessary support to both prevent side effects from developing, but also minimise their impact should they occur. All patients will have access to support groups, counselling/talking therapies, and rehabilitation programs if so desired or needed. Dieticians, physiotherapists and occupational therapists will be consulted during treatment. These can be invaluable resources for patients and their families.
Conclusion
While the prospect of long-term side effects from radiotherapy can be daunting, it’s important to balance these concerns with the benefits of treating lung cancer effectively. With ongoing advancements in radiotherapy technology and techniques, the risk of severe side effects continues to decrease. We are committed to providing the safest and most effective treatment options, ensuring that you receive the best possible care tailored to your individual needs.
Regular follow-ups, a focus on symptom management, and the use of cutting-edge technology help us minimise side effects and support you through your recovery journey and help you return to your normal life after treatment. If you have any concerns about radiotherapy or its potential long-term effects, please don’t hesitate to reach out. We are here to help every step of the way.
Remember, every patient’s journey is unique, and we are dedicated to ensuring yours is as smooth and comfortable as possible. We will offer you the right treatment, at the right time in a way that is personalised to your individual needs.
Contact us on +44 (0)20 7993 6716 to discuss how I can help you receive the best treatment for lung cancer – to eradicate the tumour, while minimising long-term side effects.
Nothing triggers my imposter syndrome more than planning post-operative radiotherapy for thymoma! As mentioned in a previous post, it really is an art – and like all art, it’s subjective.
However, two key papers help reassure me. The work of Florit Marcuse highlights the importance of collaborative working, while Andreas Rimner‘s research shows that in experienced hands, post-operative radiotherapy for thymoma does a good job! In-field recurrences are rare (as I see in my own practice).
When it comes to rare cancers like thymoma, selecting a radiation oncologist who treats patients with this condition regularly is essential. Repetition builds pattern recognition, making something rare routine.
Marcuse F et al. Radiotherapy and Oncology. 2021;165:8-13
Rimner A et al. Journal of Thoracic Oncology. 2014;9(3):403-9
Stereotactic Ablative Radiotherapy (SABR) is a cutting-edge treatment for lung cancer that delivers highly precise radiation therapy to tumours in the lungs. Unlike traditional radiation therapy, which may require numerous sessions, SABR delivers a concentrated dose of radiation in just a few sessions, often as few as one to five.
During SABR, advanced imaging techniques are used to precisely locate the tumour in the lung. The radiation beams are then carefully directed at the tumour from multiple angles, ensuring that the cancer cells receive a high dose of radiation while minimising exposure to surrounding healthy tissue.
SABR is an excellent option for patients with early-stage lung cancer who may not be candidates for surgery due to other medical issues. It offers a non-invasive alternative that can effectively destroy cancer cells while preserving lung function.
Overall, SABR is a targeted and efficient treatment option for lung cancer, offering patients hope for better outcomes with minimal impact on their daily lives.
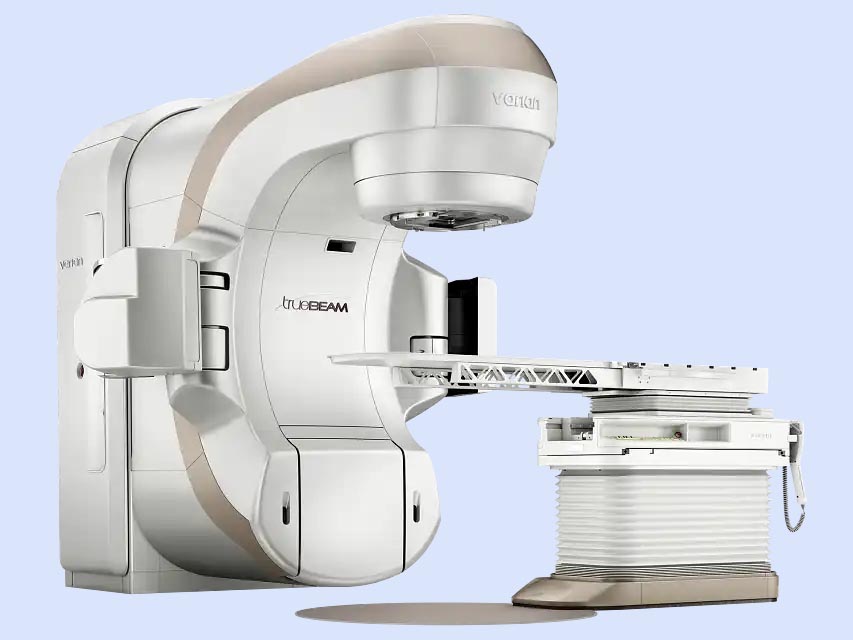
How is SABR for lung cancer given?
SABR for lung cancer is typically administered using cutting-edge treatment machines like linear accelerators (Linacs) or CyberKnife systems. These advanced devices offer precise targeting capabilities, minimising radiation exposure to healthy tissues while effectively treating the tumour. LINACs, widely used for SABR, employ high-energy X-ray beams shaped to match the tumour’s contours from various angles. The CyberKnife systems utilise robotic technology to deliver radiation beams with exceptional accuracy from multiple directions. Both LINACs and CyberKnife systems can deliver the high radiation doses necessary for SABR while prioritising patient safety and comfort.

CyberKnife and Linacs can be used for SABR
How are central lung tumours different?
Central lung tumours pose unique challenges due to their proximity to critical structures like the trachea and main bronchi. However, recent advancements in radiotherapy techniques have paved the way for more precise and targeted treatments, minimising, but not eliminating, the risk of collateral damage to healthy tissue.
Conclusion
As the landscape of cancer care continues to evolve, SABR remains a cornerstone of modern oncology, offering new hope and possibilities for patients facing lung cancer treatment.
Any questions?
Call me on 020 7993 6716 or email Carol to set up on appointment at info@drjameswilson.co.uk
Essential reading:
Tekatli H, Giraud N, van Eekelen R, Lagerwaard FJ, Senan S. Ten years outcomes after SABR in central and ultracentral primary lung tumors. Radiotherapy and Oncology. 2023;188:109848.