Non-Small Cell Lung Cancer: A Comprehensive Guide
Learn the key facts about non-small cell lung cancer, including early symptoms, risk factors, and modern treatment options.
Discover how diagnosis and staging affect prognosis — and why early detection matters.
Written by lung cancer specialist Dr James Wilson, this guide supports informed decisions.


Jump to:
- Key Takeaways
- Introduction to Non-Small Cell Lung Cancer
- What is Non-Small Cell Lung Cancer?
- Types of Non-Small Cell Lung Cancer
- Adenocarcinoma
- Squamous Cell Carcinoma
- Large Cell Carcinoma
- Other Subtypes
- Symptoms and Early Detection
- Common Symptoms of NSCLC
- The Importance of Early Detection
- Causes and Risk Factors
- Smoking: The Primary Risk Factor
- Other Risk Factors for NSCLC
- Diagnosis and Staging
- Diagnostic Tests for NSCLC
- Understanding the Staging System
- Stage 0 and Occult NSCLC
- Stages I and II
- Stages III and IV
- Treatment Options for Non-Small Cell Lung Cancer
- Surgical Treatments
- Chemotherapy for NSCLC
- Radiation Therapy Options
- Targeted Therapy: Personalised Treatment
- Immunotherapy: Boosting the Immune System
- Participating in Clinical Trials
- Living with Non-Small Cell Lung Cancer
- Managing Treatment Side Effects
- Support and Resources for Patients
- Coping Strategies and Emotional Support
- Latest Research and Breakthroughs in NSCLC
- New Treatments and Therapies on the Horizon
- Ongoing Clinical Trials and How to Participate
- Prognosis and Survival Rates
- Differences Between Small Cell and Non Small Cell Lung Cancer
- UK-Specific Healthcare Considerations
- Conclusion
- Next Steps for Personalised Care
- Frequently Asked Questions About Non-Small Cell Lung Cancer
- What are the different stages of NSCLC?
- How is NSCLC typically treated?
- What is the prognosis for someone with NSCLC?
- Are there screening tests for NSCLC?
- How can I reduce my risk of developing NSCLC?
- Get Personalised Advice About Your Diagnosis
Key Takeaways
-
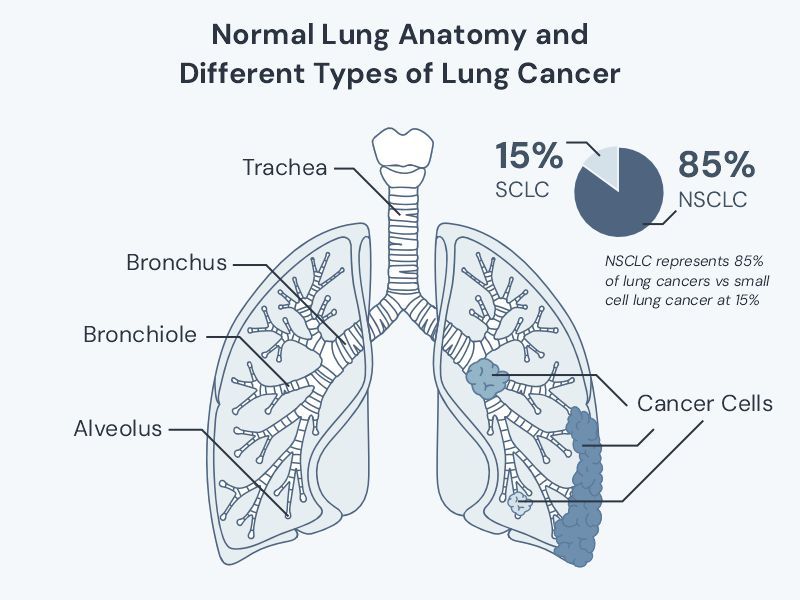
Non small cell lung cancer accounts for approximately 85% of all lung cancer cases, making it the most common type compared to small cell lung cancer
-
Early detection through chest x-ray and CT scan significantly improves survival rates and treatment options
-
Modern treatment approaches including targeted therapy, immunotherapy, and precision medicine offer hope even for advanced-stage disease
-
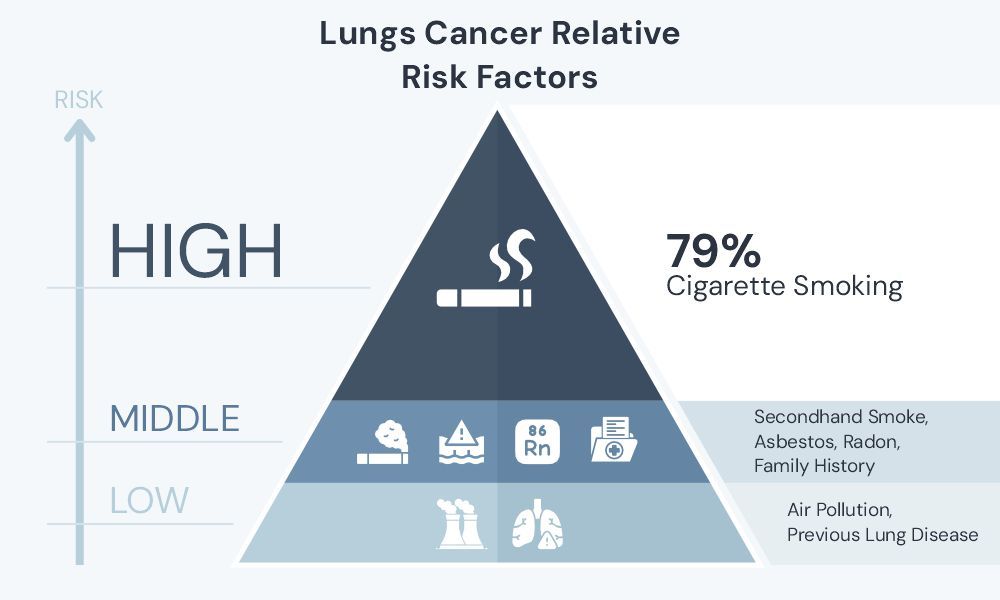
Risk factors include cigarette smoke, secondhand smoke, family history, and environmental exposures like asbestos
-
According to Cancer Research UK, 79% of lung cancer cases are preventable, highlighting the importance of risk reduction
To receive a comprehensive guide to lung cancer to your email, please register here.
Introduction to Non-Small Cell Lung Cancer
Non small cell lung cancer represents the vast majority of primary lung cancer diagnoses worldwide. According to Cancer Research UK, there were 49,229 new cases of lung cancer diagnosed between 2017-2019 in the UK, with non small cell lung cancer accounting for approximately 85% of these cases. As an oncologist specialising in thoracic malignancies, I see patients with this condition daily across my clinics in London.
The distinction between small cell lung cancer and non small cell lung cancer is fundamental to understanding your diagnosis and treatment options. While both types can be serious, small cell lung cancer and non small cell lung cancer behave very differently and require distinct treatment approaches.
Understanding your type of cancer is the first step towards making informed decisions about your care. This comprehensive guide will provide general information and will walk you through everything you need to know about non small cell lung cancer, from the basic biology to the latest treatment breakthroughs.
What is Non-Small Cell Lung Cancer?
Non small cell lung cancer develops when normal cells in the lung undergo DNA damage and begin to divide uncontrollably. The key difference between small cell and non small cell lung cancer lies in how the cancer cells appear under microscopic examination and how they behave clinically.
Non-small-cell lung cancer tends to grow more slowly than small cell lung cancer, though this varies significantly between individuals. The cancer cells arise from epithelial cells that line the airways and tiny air sacs called alveoli. These cells normally help exchange oxygen and carbon dioxide, but when they become cancerous, they lose their normal function and begin forming tumours.
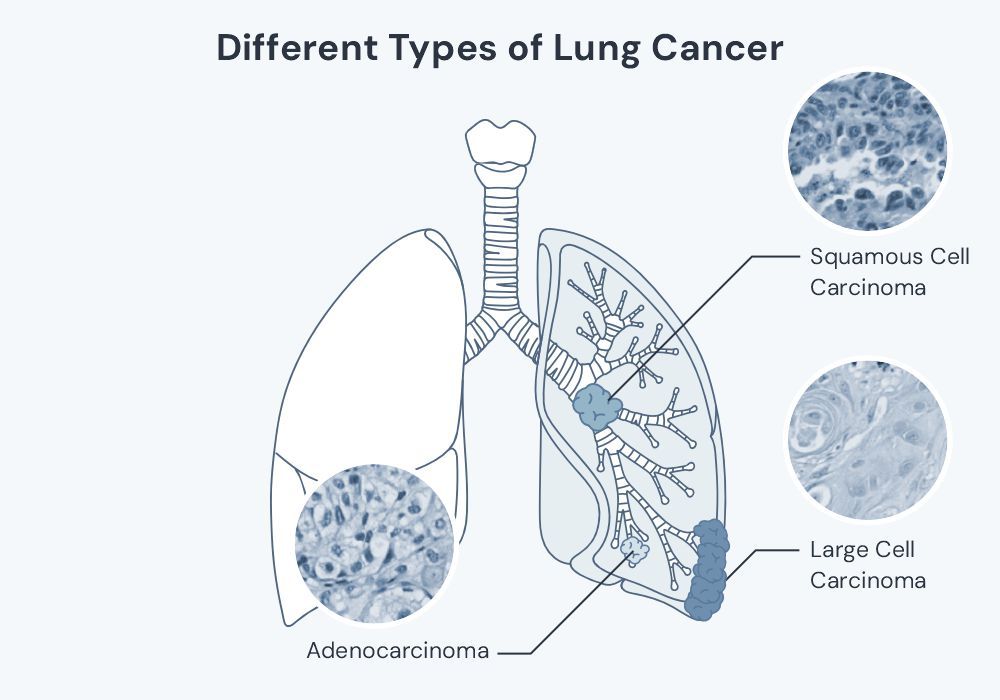
Understanding what is non small cell lung cancer requires recognising that this category encompasses several distinct subtypes, each with unique characteristics. The main types of non small cell lung cancer include adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Small cell vs non small cell lung cancer represents one of the most important distinctions in lung cancer classification. This difference affects everything from treatment selection to prognosis, making accurate diagnosis crucial for optimal care. Both types of lung cancer can occur in any part of the lung as can rare lung cancers such as carcinoid tumours.
Types of Non-Small Cell Lung Cancer
Adenocarcinoma
Adenocarcinoma represents the most common type of non small cell lung cancer, accounting for approximately 40% of all lung cancer diagnoses. This cancer type typically develops in the outer areas of the lung and often affects non-smokers more frequently than other types of non small cell lung cancer.
Adenocarcinoma includes several subtypes, including adenosquamous carcinoma, which shows characteristics of both adenocarcinoma and squamous cell carcinoma. This rare subtype requires careful pathological examination to guide appropriate treatment selection.
The cancer cells in adenocarcinoma often show specific genetic mutations, particularly in the epidermal growth factor receptor (EGFR) and Anaplastic Lymphoma Kinase (ALK) genes. These genetic changes have revolutionised treatment, as we can now use targeted therapies designed specifically for these molecular alterations.
Squamous Cell Carcinoma
Squamous cell carcinoma typically develops in the central portions of the lung, often near the main airways. This type accounts for approximately 25-30% of non small cell lung cancer cases and shows a strong association with cigarette smoking.
The cancer cells arise from the flat, scale-like cells that line the airways. These cells normally help protect the lung from inhaled irritants, but chronic exposure to carcinogens can cause them to become malignant.
Squamous cell carcinoma tends to remain localised longer than adenocarcinoma before spreading to lymph nodes or distant organs. This characteristic can sometimes allow for earlier detection and more successful surgical treatment.
Large Cell Carcinoma
Large cell carcinoma represents the least common major subtype of non small cell lung cancer, comprising roughly 10-15% of cases. Large cell lung cancer gets its name from the appearance of the cancer cells under microscopic examination.
These tumours can develop anywhere in the lung and tend to grow and spread rapidly. The cancer cells are large and poorly differentiated, meaning they don't closely resemble normal lung tissue.
Other Subtypes
Several less common subtypes of non small cell lung cancer deserve mention. Carcinoid tumours represent a unique category that typically grows more slowly and may produce hormones that cause specific symptoms.
Other rare subtypes include sarcomatoid carcinomas and various mixed histologies. Each subtype requires individualised treatment approaches based on specific characteristics and molecular features.
Symptoms and Early Detection
Common Symptoms of NSCLC
The symptoms of lung cancer can vary significantly depending on the location and size of the tumour. Understanding signs of non small cell lung cancer helps patients seek timely medical evaluation when concerning symptoms develop.
Chest pain represents one of the most common presenting symptoms of non small cell lung cancer. This chest pain may feel sharp, dull, or aching, and often worsens with deep breathing or coughing. The chest pain typically occurs because the tumour affects the chest wall or pleural lining around the lung.
A persistent cough that doesn't resolve after several weeks should always be evaluated, particularly in individuals with risk factors for lung cancer. The cough may be dry or produce sputum, sometimes with blood-tinged secretions.
Weight loss often occurs as the cancer progresses, even when patients maintain normal appetite. This weight loss happens because cancer cells consume significant energy and may interfere with normal metabolism.
Shortness of breath develops when tumours block major airways or when fluid accumulates around the lung. Patients may notice they become winded more easily during normal activities.
Bone pain can signal that the cancer has spread beyond the lung to the skeletal system. This bone pain is often worse at night and may not respond well to standard pain medications.
Non small cell lung cancer symptoms may also include fatigue, hoarseness, and recurrent respiratory infections. These symptoms can be subtle initially, which is why many patients receive their diagnosis at advanced stages.
The Importance of Early Detection
Early detection dramatically improves survival rates for patients with non small cell lung cancer. When we catch the disease in early-stage forms, surgical resection often provides the best chance for cure, with survival rates significantly higher than those seen in advanced disease.
Unfortunately, many patients receive their diagnosis only after the cancer has reached advanced stages. This happens because early-stage non small cell lung cancer often produces no noticeable symptoms until the tumour grows significantly.
Screening programmes using low-dose CT scanning can detect lung cancers before symptoms develop. These programmes target high-risk individuals, particularly those with significant smoking histories, and can identify small nodules that might not be visible on standard chest x-ray imaging.
According to Cancer Research UK data, only 10% of people diagnosed with lung cancer survive for 10 or more years, but survival rates are much higher when the disease is caught early. Early detection represents our best opportunity to improve these statistics.
Causes and Risk Factors
Understanding the risk factors for non small cell lung cancer helps individuals make informed decisions about screening and lifestyle modifications that may reduce their cancer risk.
Smoking: The Primary Risk Factor
Cigarette smoking remains the most important risk factor for developing non small cell lung cancer. The relationship between cigarette smoke and lung cancer is well-established, with smokers facing a 15-20 fold increased risk compared to never-smokers.
The risk correlates directly with both the number of cigarettes smoked daily and the total duration of smoking. Heavy smokers who consume multiple packs daily face the highest risk, but even light smoking significantly increases cancer risk.
According to Cancer Research UK, 79% of lung cancer cases are preventable, with smoking being the primary preventable cause. This statistic highlights the enormous potential impact of smoking cessation programmes.
The good news is that quitting smoking at any age reduces lung cancer risk. Former smokers see their risk decrease gradually over time, though it may take 15-20 years to approach the levels seen in never-smokers.
E-cigarettes and vaping products also carry potential risks, though the long-term cancer effects remain under investigation. The safest approach is to avoid all tobacco and nicotine products.
Other Risk Factors for NSCLC
Secondhand smoke exposure creates a real cancer risk for non-smokers. Family members and coworkers of smokers face increased lung cancer risk due to environmental tobacco smoke exposure, demonstrating that cigarette smoke affects even those who don't smoke directly.
Family history plays a role in lung cancer development, suggesting genetic susceptibility factors. Individuals with close relatives who developed lung cancer may face higher risk even without smoking, indicating that family history represents an important risk factor to consider.
There is growing evidence of a link between ultra-processed food and lung cancer.
Environmental and occupational exposures contribute to lung cancer risk. Asbestos exposure, particularly in construction and shipbuilding industries, significantly increases cancer risk. The combination of asbestos exposure and smoking creates especially high risk.
Radon gas exposure in homes represents another important risk factor. This naturally occurring radioactive gas can accumulate in basements and lower floors of buildings, creating long-term exposure risks.
Air pollution, particularly in urban areas with heavy traffic, may contribute to lung cancer development. Fine particulate matter and diesel exhaust contain carcinogenic compounds that may increase the risk of lung cancer.
Previous lung diseases, including pulmonary fibrosis and chronic obstructive pulmonary disease, may increase lung cancer risk. The chronic inflammation associated with these conditions may contribute to cancer development through ongoing tissue damage.
Diagnosis and Staging
Diagnostic Tests for NSCLC
When lung cancer is suspected, several diagnostic tests help confirm the diagnosis and determine the extent of disease. The diagnostic process typically begins with clinical assessment including physical examination, imaging studies and progresses to tissue sampling for definitive diagnosis.
A chest x-ray often provides the first clue about possible lung cancer. While a chest x-ray can detect larger tumours, it may miss smaller cancers or those hidden behind other structures like the heart or ribs. However, a chest x-ray remains an important initial screening tool due to its accessibility and low cost.
CT scan (computed tomography) of the chest provides much more detailed images than standard chest x-ray imaging. A CT scan can detect smaller nodules and better evaluate lymph nodes throughout the chest. Most non small cell lung cancer diagnoses rely on CT scan findings for initial assessment, making this imaging study crucial for proper evaluation.
Positron emission tomography, commonly called a PET scan, uses radioactive glucose to identify areas of high metabolic activity typical of cancer cells. PET scans help determine whether suspicious areas represent cancer and whether the disease has spread beyond the lung.
Magnetic resonance imaging of the brain is often performed to check for brain metastases, particularly in patients with adenocarcinoma or advanced disease. This imaging helps complete the staging process for treatment planning.
Bone scan may be recommended to evaluate for bone metastases, especially in patients with bone pain or elevated blood markers suggesting skeletal involvement. A bone scan can detect cancer spread to bones before symptoms develop.
Medical tests also include various blood tests to assess general health and look for tumour markers. While blood tests cannot diagnose lung cancer directly, they provide important information about overall health and organ function.
Tissue sampling remains essential for confirming the diagnosis and determining the specific type of non small cell lung cancer. This may involve bronchoscopy, where a flexible scope is passed through the mouth into the airways to obtain tissue samples.
For tumours that cannot be reached through bronchoscopy, CT-guided needle biopsy may be performed. This surgical procedure uses CT scan guidance to place a needle through the chest wall to sample the tumour.
Genetic testing of the tumour tissue has become standard practice. This testing looks for specific mutations like EGFR and ALK that can guide targeted therapy decisions, representing a crucial component of modern cancer care.
Understanding the Staging System
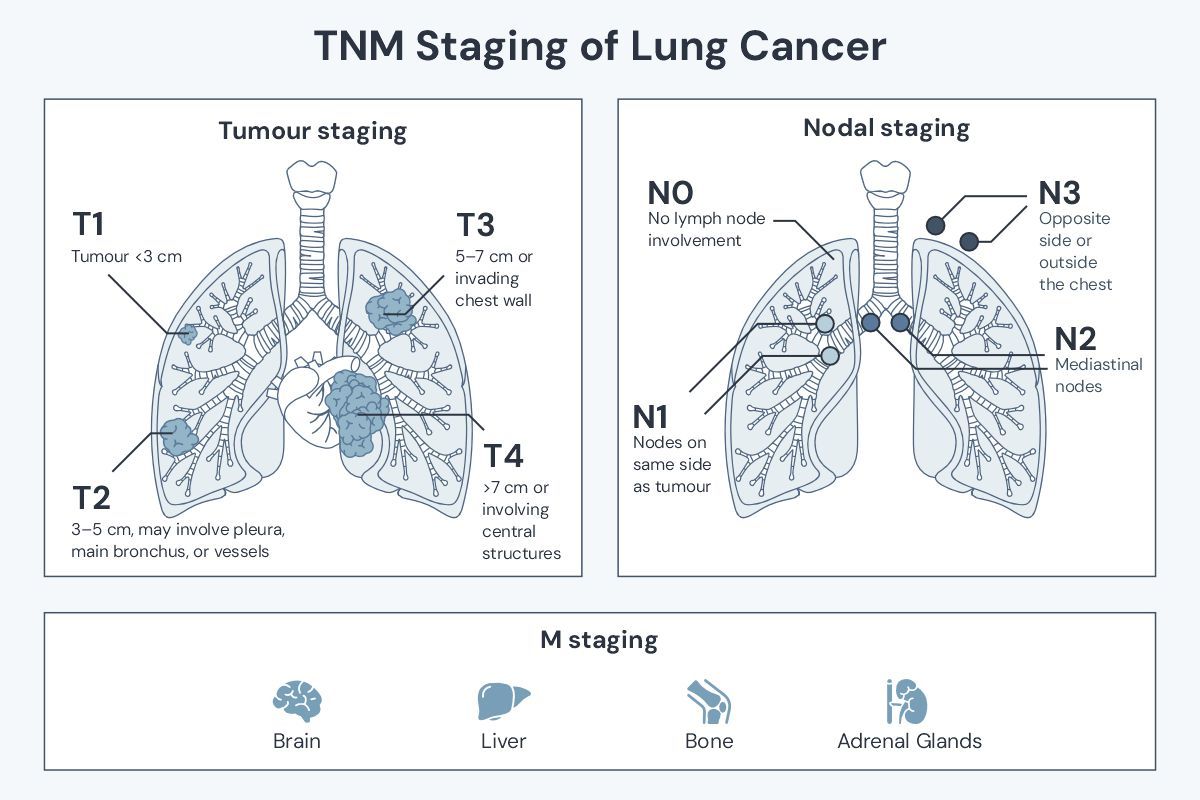
Staging describes the extent of cancer spread and helps guide treatment decisions. The staging system for non small cell lung cancer uses the TNM classification, which evaluates the primary tumour (T), lymph nodes (N), and distant metastases (M).
The TNM information is combined to assign an overall stage from 0 to IV. Understanding the stage of the cancer helps predict prognosis and guides treatment recommendations for optimal outcomes.
Stage 0 and Occult NSCLC
Stage 0 represents carcinoma in situ, where abnormal cells are present but haven't spread to nearby tissue. This very early stage has an excellent prognosis with appropriate treatment, often achieving cure rates exceeding 95%.
Occult lung cancer refers to cases where cancer cells are found in sputum but no tumour can be located with imaging studies. This unusual situation requires careful evaluation and monitoring.
Stages I and II
Early-stage disease includes stages I and II, where the cancer remains localised to the lung with no or limited lymph node involvement. These stages represent the best opportunity for curative treatment.
Stage I tumours are smaller (typically less than 3-4 centimetres) and haven't spread to lymph nodes. These cancers often can be treated with surgical resection alone, offering excellent cure rates with five-year survival rates exceeding 70-80%.
Stage II disease involves slightly larger tumours or limited spread to nearby lymph nodes. Treatment typically includes surgery followed by adjuvant chemotherapy to reduce recurrence risk and improve long-term outcomes.
The survival rate for early-stage non small cell lung cancer is encouraging, particularly when compared to more advanced disease stages. Early detection through screening programmes aims to identify more cancers at these treatable stages.
Stages III and IV
Advanced-stage disease includes stages III and IV, representing more extensive cancer spread that requires multimodal treatment approaches.
Stage III encompasses locally advanced disease where the cancer has spread to lymph nodes in the centre of the chest or has grown into nearby structures. This stage often requires multimodal treatment combining surgery, radiation therapy, and systemic therapy.
Stage IV represents metastatic disease where cancer has spread to distant organs. Common sites include the brain, liver, bones, and adrenal gland. While stage IV disease is more challenging to treat, many patients achieve significant benefit from modern therapies.
According to Cancer Research UK data, survival rates vary significantly by age, with almost a third (29.0%) of people diagnosed aged 15-44 surviving their disease for ten years or more, compared with 4.6% of people diagnosed aged 75-99.
The treatment approach for advanced-stage disease has evolved dramatically in recent years. Combination treatments and new targeted therapies offer hope even for patients with extensive disease.
Treatment Options for Non-Small Cell Lung Cancer
Treatment for non small cell lung cancer requires individualised planning based on multiple factors including stage, molecular characteristics, and overall health. I work with each patient to develop a comprehensive treatment plan that addresses their specific situation and maximises their chances of the best treatment outcomes.
Surgical Treatments
Surgical resection offers the best chance for cure in patients with early-stage non small cell lung cancer. The surgical procedure depends on tumour location, size, and the patient's lung function and general health.
Lobectomy represents the standard surgical approach for most early-stage cancers. This surgical procedure removes the entire lobe of the lung containing the tumour along with associated lymph nodes, providing excellent local control.
Segmentectomy or wedge resection may be appropriate for smaller tumours or patients with limited lung function. These procedures remove smaller portions of the lung while preserving more healthy tissue.
Pneumonectomy, removal of an entire lung, is sometimes necessary for larger tumours that involve central structures. This major surgical procedure requires careful patient selection and thorough preoperative evaluation.
Video-assisted thoracoscopic surgery (VATS) allows many procedures to be performed through smaller incisions, reducing recovery time and postoperative discomfort. This minimally invasive approach is suitable for many early-stage tumours.
Thoracic surgery requires expertise in managing complex cases and potential complications. The surgical team includes specialists in anaesthesia, critical care, and rehabilitation to ensure optimal outcomes.
Chemotherapy for NSCLC
Chemotherapy for non small cell lung cancer uses drugs that target rapidly dividing cancer cells throughout the body. For non small cell lung cancer, chemotherapy may be used before surgery (neoadjuvant therapy), after surgery (adjuvant chemotherapy), or as primary treatment for advanced disease.
Adjuvant chemotherapy following surgical resection reduces the risk of cancer recurrence. This treatment is typically recommended for patients with stage II or III disease who have recovered well from surgery.
Neoadjuvant therapy given before surgery can shrink tumours and potentially improve surgical outcomes. This approach is often used for locally advanced disease where immediate surgery might not be feasible.
For advanced disease, chemotherapy for non small cell lung cancer serves as a cornerstone of treatment. Modern chemotherapy regimens are more effective and better tolerated than older treatments.
Combination chemotherapy typically uses two or more drugs that work through different mechanisms. Common combinations include platinum-based drugs with newer agents that target specific cellular processes.
Radiation Therapy Options
Radiation therapy uses high-energy beams to destroy cancer cells while minimising damage to healthy tissue. Modern radiation therapy techniques allow precise targeting of tumours while sparing normal organs.
External beam radiation therapy represents the most common approach for lung cancer. Advanced techniques like intensity-modulated radiation therapy (IMRT) and stereotactic body radiation therapy (SBRT) provide excellent tumour control with reduced side effects.
For early-stage disease in patients who cannot undergo surgery, SBRT offers an excellent alternative. This technique delivers high doses of radiation therapy in just a few treatments, achieving cure rates comparable to surgery in selected patients. SABR also plays in role in the treatment of secondary lung cancer.
Radiation therapy often combines with chemotherapy for locally advanced disease. This combined approach, called chemoradiotherapy, can improve outcomes compared to either treatment alone. Proton beam therapy plays a role, particularly in the treatment of previously treated non-small cell lung cancer.
Targeted Therapy: Personalised Treatment
Targeted therapy represents one of the most exciting advances in non small cell lung cancer treatment. These drugs specifically target molecular abnormalities found in cancer cells, offering more precise treatment approaches.
EGFR mutations occur in approximately 10-15% of lung adenocarcinomas, particularly in non-smokers and women. Patients with EGFR mutations often respond dramatically to targeted drugs like erlotinib, gefitinib, or osimertinib.
ALK rearrangements affect roughly 3-5% of lung adenocarcinomas, typically in younger patients with minimal smoking history. ALK inhibitors like crizotinib, alectinib, and brigatinib provide excellent disease control for these patients.
Other targetable mutations include ROS1, BRAF, and MET alterations. As our understanding of cancer genetics expands, new targeted therapies continue to emerge for different types of non small cell lung cancer.
Genetic testing of tumour tissue is essential to identify patients who may benefit from targeted therapy. This testing should be performed on all patients with advanced adenocarcinoma and selected patients with other histologies.
Immunotherapy: Boosting the Immune System
Immunotherapy works by enhancing the immune system's ability to recognise and destroy cancer cells. These treatments have revolutionised care for many patients with advanced non small cell lung cancer.
Immune checkpoint inhibitors like pembrolizumab, nivolumab, and atezolizumab block proteins that prevent immune cells from attacking cancer. These drugs can provide durable responses in selected patients with non small cell lung cancer.
PD-L1 expression testing helps identify patients most likely to benefit from immunotherapy. Patients with high PD-L1 expression often achieve excellent responses to single-agent immunotherapy.
Combination immunotherapy approaches may benefit patients with lower PD-L1 expression. Combining checkpoint inhibitors with chemotherapy or other immunotherapy drugs can improve response rates.
Participating in Clinical Trials
Ongoing clinical trials offer access to the newest treatments before they become widely available. Clinical trials are essential for advancing cancer care and may provide excellent treatment options for appropriate patients.
Trials may investigate new drugs, new combinations of existing treatments, or new approaches to radiation therapy or surgery. Participation in trials is voluntary and includes additional monitoring and safety measures.
I regularly discuss clinical trial opportunities with my patients, particularly those with advanced disease or uncommon molecular features. Many of today's standard treatments for non small cell lung cancer were developed through clinical trials.
Living with Non-Small Cell Lung Cancer
A diagnosis of non small cell lung cancer affects every aspect of life, from physical health to emotional wellbeing. Learning to live with cancer involves adapting to new challenges while maintaining quality of life throughout the treatment journey.
Managing Treatment Side Effects
Modern cancer treatments are generally better tolerated than older therapies, but side effects can still impact daily life. Understanding potential side effects and management strategies helps patients prepare for treatment.
Fatigue represents one of the most common side effects across all treatment types. This cancer-related fatigue differs from normal tiredness and may not improve with rest alone. Gentle exercise, good nutrition, and stress management can help combat fatigue.
Nausea and appetite changes often accompany chemotherapy and radiation therapy. Anti-nausea medications have improved significantly, and working with a nutritionist can help maintain adequate nutrition during treatment.
Skin reactions may occur with radiation therapy, typically resembling sunburn in the treated area. Proper skin care and avoiding irritants can minimise discomfort during treatment.
Targeted therapies may cause specific side effects like skin rashes or diarrhoea. Most side effects are manageable with appropriate medications and monitoring.
Immunotherapy can cause unique side effects related to immune system activation. While generally well-tolerated, these treatments require careful monitoring for autoimmune reactions.
Support and Resources for Patients
Cancer care extends far beyond medical treatment to include comprehensive support services. A strong support network significantly improves treatment outcomes and quality of life for cancer patients.
Support groups connect patients with others facing similar challenges. Many patients find comfort in sharing experiences and learning from others who understand their situation with non small cell lung cancer.
Local support services may include transportation assistance, meal programmes, and financial counselling. Many cancer centres offer these services to help patients focus on their health rather than logistical challenges.
Mental health support is crucial for patients and families dealing with cancer. Professional counselling can help process emotions and develop coping strategies for the challenges ahead.
Palliative care focuses on symptom management and quality of life throughout the cancer journey. This specialised care complements cancer treatment and can begin at any stage of illness.
Coping Strategies and Emotional Support
Emotional responses to cancer diagnosis vary widely, and all feelings are valid. Common reactions include fear, anger, sadness, and uncertainty about the future, particularly given the survival statistics for lung cancer.
Maintaining normal activities when possible helps preserve quality of life and emotional wellbeing. This might mean continuing work, hobbies, or social activities as energy and general health permit.
Communication with family and friends becomes especially important. Honest conversations about needs, fears, and hopes help build stronger support networks during treatment.
Stress management techniques like meditation, deep breathing, or gentle exercise play a major role in managing anxiety and improve overall wellbeing. Many patients find benefit in practices like yoga or tai chi.
Professional mental health support may be helpful, particularly during difficult treatment periods or when facing challenging decisions about care.
Latest Research and Breakthroughs in NSCLC
The field of lung cancer treatment continues to evolve rapidly, with new discoveries leading to improved outcomes for patients with non small cell lung cancer. Staying informed about research developments helps patients understand their options and maintain hope for the future.
New Treatments and Therapies on the Horizon
Precision medicine continues to expand in medical oncology with the discovery of new targetable mutations. Researchers regularly identify genetic alterations that drive cancer growth and develop corresponding targeted therapies for different types of non small cell lung cancer.
Combination approaches show promise for improving treatment outcomes. Studies investigate optimal ways to combine immunotherapy, targeted therapy, and traditional treatments like chemotherapy and radiation therapy.
Liquid biopsies represent an emerging technology that can detect cancer DNA in blood samples. This approach may allow earlier detection of recurrence and monitoring of treatment response without invasive procedures.
Artificial intelligence and machine learning are being applied to improve treatment selection and predict treatment outcomes. These technologies may help personalise treatment decisions even further for individual cancer patients.
Novel drug delivery systems aim to improve how medications reach cancer cells while reducing side effects. These approaches include targeted nanoparticles and local delivery methods.
Ongoing Clinical Trials and How to Participate
Clinical trials remain essential for advancing lung cancer treatment. Current studies investigate treatments across all stages of disease, from early detection to advanced therapeutics for non small cell lung cancer.
Prevention trials study whether certain interventions can reduce lung cancer risk in high-risk individuals. These might include chemoprevention agents or enhanced screening approaches.
Treatment trials investigate new drugs, drug combinations, or treatment sequences. These studies often focus on specific patient populations or molecular subtypes of non small cell lung cancer.
Quality of life trials examine ways to improve patient experiences during treatment. These studies might investigate supportive care interventions or rehabilitation programmes.
Participation in clinical trials requires meeting specific eligibility criteria and understanding potential risks and benefits. The research team provides detailed information to help patients make informed decisions.
Many trials are available through major cancer centres like those where I practice in London. National Cancer Institute resources also provide information about trials throughout the UK and internationally.
Prognosis and Survival Rates
Understanding non small cell lung cancer prognosis helps patients and families prepare for the journey ahead while maintaining realistic hope. Survival rates vary significantly based on multiple factors, including stage at diagnosis, age, overall health, and molecular characteristics.
According to Cancer Research UK, overall lung cancer survival statistics show that 10% of people survive lung cancer for 10 or more years. However, survival rates for non small cell lung cancer vary dramatically by stage, with early-stage disease offering much better outcomes.
Non small cell lung cancer survival rates are notably higher for younger patients. Cancer Research UK data shows that almost a third (29.0%) of people diagnosed aged 15-44 survive their disease for ten years or more, compared with just 4.6% of people diagnosed aged 75-99.
The non small cell lung cancer prognosis has improved modestly over recent decades, though progress has been slower than for some other cancer types. According to Cancer Research UK, in the 1970s, less than 5 in 100 (3.1%) people diagnosed with lung cancer survived beyond ten years, while by the 2010s this had increased to 5 in 100 (4.9%).
Socioeconomic factors also influence survival outcomes. Cancer Research UK reports that a quarter (25.3%) of people in the least deprived group survive their disease for five years or more, compared with 18.2% of people in the most deprived group.
For patients with specific molecular alterations like EGFR mutations or ALK rearrangements, targeted therapies have significantly improved survival outcomes. These patients often achieve much better prognosis than historical averages suggest.
Life expectancy with non small cell lung cancer depends heavily on stage at diagnosis. Early-stage disease offers the possibility of cure, while advanced disease focuses on extending life and maintaining quality of life through effective treatments.
Differences Between Small Cell and Non Small Cell Lung Cancer
Understanding the difference between small cell and non small cell lung cancer is crucial for patients and families navigating a lung cancer diagnosis. These two main types of lung cancer behave very differently and require distinct treatment approaches.
Small cell lung cancer versus non small cell lung cancer differs in several key ways. Small cell lung cancer grows and spreads much more rapidly than non small cell lung cancer, often spreading to distant organs before diagnosis.
The difference between small cell lung cancer and non small cell lung cancer also extends to treatment options. Small cell lung cancer typically responds better to chemotherapy and radiation therapy but is less likely to be curable with surgery.
Small cell vs non small cell lung cancer also differs in terms of smoking association. While both types are linked to smoking, small cell lung cancer shows an even stronger association with cigarette smoking than non small cell lung cancer.
Non small cell lung cancer versus small cell lung cancer also differs in terms of molecular targets. Non small cell lung cancer is more likely to have targetable genetic mutations that can be treated with specific targeted therapies.
When comparing small cell lung cancer vs non small cell lung cancer survival rates, non small cell lung cancer generally offers better long-term survival, particularly for early-stage disease. However, small cell lung cancer may respond more dramatically to initial treatment.
The staging systems also differ between small cell and non small cell lung cancer. Small cell lung cancer uses a simpler two-stage system (limited vs extensive disease), while non small cell lung cancer uses the more detailed TNM staging system.
Small cell lung cancer and non small cell lung cancer prognosis varies significantly. While small cell lung cancer may respond well initially, it has a higher tendency to recur and develop resistance to treatment.
UK-Specific Healthcare Considerations
Accessing care for non small cell lung cancer in the UK involves navigating both NHS and private healthcare options. Understanding the healthcare landscape helps patients make informed decisions about their care.
The NHS provides comprehensive cancer services across the UK, including diagnosis, staging, and treatment for non small cell lung cancer. NHS guidelines follow evidence-based protocols to ensure consistent, high-quality care.
Referral pathways typically begin with GP consultation for concerning symptoms like persistent cough, chest pain, or weight loss. The two-week wait rule ensures rapid specialist assessment for patients with suspected lung cancer.
Multidisciplinary team meetings bring together specialists from different disciplines to plan individualised treatment approaches. These teams include oncologists, surgeons, radiologists, and specialist nurses.
Private healthcare options may offer shorter waiting times and access to some newer treatments that may not yet be available through the NHS. However, NHS care provides comprehensive services with excellent outcomes.
Access to clinical trials represents an important consideration for many patients. Both NHS and private centres participate in research studies investigating new treatments for non small cell lung cancer.
Support services vary by region but may include specialist lung cancer nurses, social workers, and palliative care teams. Cancer charities also provide valuable support and information resources.
For patients in my care, I provide consultation services across four London locations:
-
LOC - Harley Street: 95 Harley Street, London, W1G 6AF
-
LOC - Sydney Street: 102 Sydney Street, London, SW3 6NJ
-
The London Clinic: 20 Devonshire Place, London W1G 6BW
-
The Cromwell Hospital: 164-178 Cromwell Road, London SW5 0TU
I also offer video consultations for patients throughout the UK and internationally, ensuring that geographic location doesn't limit access to specialist care.
Conclusion
Non small cell lung cancer represents a complex disease that requires comprehensive, personalised care. While the diagnosis can feel overwhelming, significant advances in treatment offer genuine hope for patients at all stages of disease.
Early detection through appropriate screening remains crucial for improving survival rates. If you have risk factors for lung cancer, particularly a smoking history, discuss screening options with your healthcare provider. Remember that Cancer Research UK data shows 79% of lung cancer cases are preventable.
Modern treatment approaches combine multiple modalities to achieve the best possible outcomes. Surgery, radiation therapy, chemotherapy for non small cell lung cancer, targeted therapy, and immunotherapy each play important roles in comprehensive cancer care.
The importance of molecular testing cannot be overstated. Understanding the genetic characteristics of your tumour opens doors to personalised treatment approaches that may be more effective and better tolerated than traditional therapies. Age should not be a barrier to treatment. I see many older people with non-small cell lung cancer for treatment.
Living with lung cancer involves more than medical treatment. Comprehensive support services, including nutritional counselling, mental health support, and practical assistance, contribute significantly to quality of life during treatment.
Research continues to advance our understanding and treatment of non small cell lung cancer. Clinical trials offer access to the newest therapies and hope for even better outcomes in the future.
Next Steps for Personalised Care
If you're facing a lung cancer diagnosis or have concerns about your risk, I encourage you to seek expert consultation. As a specialist in thoracic oncology, I provide comprehensive evaluations and treatment planning at several London locations, with video consultation options for patients unable to travel.
My approach focuses on providing hope while delivering the highest standard of evidence-based treatment. Every patient deserves comprehensive evaluation, personalised treatment planning, and ongoing support throughout their cancer journey.
Take the next step: Explore treatment options and support for non-small cell lung cancer. Contact Dr James Wilson today to discuss your individual situation and develop a personalised care plan.
Frequently Asked Questions About Non-Small Cell Lung Cancer
What are the different stages of NSCLC?
Non small cell lung cancer staging uses the TNM system to classify disease extent. Stage 0 represents carcinoma in situ with no invasion. Stages I and II indicate early disease confined to the lung with no or limited lymph node involvement, offering the best survival rates. Stage III represents locally advanced disease with significant lymph node involvement or invasion of nearby structures. Stage IV indicates metastatic disease with spread to distant organs. Each stage of the cancer guides treatment decisions and helps predict outcomes, with early-stage disease offering much better prognosis.
How is NSCLC typically treated?
Treatment for non small cell lung cancer depends on stage, molecular characteristics, and overall health. Early-stage disease often involves surgical resection followed by adjuvant chemotherapy if indicated. Locally advanced disease typically requires multimodal treatment combining chemotherapy for non small cell lung cancer, radiation therapy, and sometimes surgery. Advanced disease treatment focuses on systemic therapies including chemotherapy, targeted therapy, and immunotherapy. The specific treatment plan is individualised based on tumour genetics and patient factors, with genetic testing playing a crucial role in modern treatment decisions.
What is the prognosis for someone with NSCLC?
Non small cell lung cancer prognosis varies significantly based on stage at diagnosis and molecular characteristics. According to Cancer Research UK, overall lung cancer survival shows that 10% of people survive for 10 or more years, but survival rates are much higher for early-stage disease. Patients diagnosed aged 15-44 have a 29.0% ten-year survival rate compared to 4.6% for those aged 75-99. Five-year survival rates exceed 70-80% for stage I disease treated appropriately. Patients with targetable mutations like EGFR or ALK often achieve excellent disease control with appropriate targeted therapies. Individual prognosis depends on multiple factors that should be discussed with your oncologist.
Are there screening tests for NSCLC?
Low-dose CT scanning is recommended for high-risk individuals, typically those aged 50-80 with significant smoking history. Screening can detect lung cancers before symptoms develop, when treatment is most effective and survival rates are highest. The decision to screen should involve discussion of individual risk factors, potential benefits, and possible harms. People aged over 55 with a smoking history are invited to screening in the UK. Chest x-ray alone is not sufficient for screening, as CT scan provides much more detailed imaging for early detection.
How can I reduce my risk of developing NSCLC?
There are many different ways of reducing your NSCLC risk. Avoiding tobacco use represents the most important step for lung cancer prevention, as it plays such a major role. If you smoke, stopping at any age reduces cancer risk significantly. Avoiding secondhand smoke exposure also decreases risk factors. Testing homes for radon and addressing elevated levels when found helps reduce environmental risk. Maintaining good general health through regular exercise and a healthy diet may provide additional protection. For individuals with occupational exposures like asbestos, following safety guidelines and regular health monitoring are important for reducing lung cancer risk.
Get Personalised Advice About Your Diagnosis
Even if you’re still processing your diagnosis or waiting on tests, early advice can make a real difference.
I offer consultations within 24–48 hours – with no GP referral required.
You can call 020 7993 7616, email info@drjameswilson.co.uk, or submit the contact form here to begin.
Cancer doesn’t wait. Neither should you.