Can a Lung Nodule Be Cancer?
If a scan shows a lung nodule, it is completely normal to feel anxious. Most people hear the word “nodule” and their brain goes straight to the worst-case scenario.


Jump to:
The reassuring bit is this: Lung nodules are common, and most are not cancer. A small number are, which is why we take them seriously, but we do not have to panic. We just need a sensible plan.
In this article, I will explain what lung nodules are, what makes one more or less worrying, how we usually investigate them, and what to do next.
What is a lung nodule?
A lung nodule is a small, round (or slightly irregular) spot in the lung, usually found by accident on a chest X-ray or CT scan done for something else.
Most nodules cause no symptoms at all. People often only know about them because the scan picked them up.
You will sometimes hear clinicians use slightly different wording, but broadly:
-
A nodule is usually considered something under 3 cm
-
Anything larger may be described as a mass, which tends to raise concern and usually needs a faster work-up
The key point is that a nodule is a finding, not a diagnosis. The job is to work out what it represents.
What causes lung nodules?
The most common causes are benign, and often relate to old inflammation in the lung, for example:
-
Previous infections (including old healed infections you might not even remember)
-
Prior tuberculosis exposure (still relevant in the UK, depending on background and history)
-
Inflammatory or autoimmune conditions (such as rheumatoid arthritis)
-
Long-term exposure to dusts or irritants (certain workplaces can matter here)
Less commonly, a nodule can be cancer, either:
-
A primary lung cancer
-
A cancer that has spread to the lung from elsewhere
Smoking does not directly “create” nodules, but it does increase the chance that a nodule could be malignant. That is why your smoking history matters so much in risk assessment.
How likely is it to be cancer?
Most lung nodules are not cancer. In practice, a big part of my role is turning vague fear into a clearer estimate of risk, based on the details.
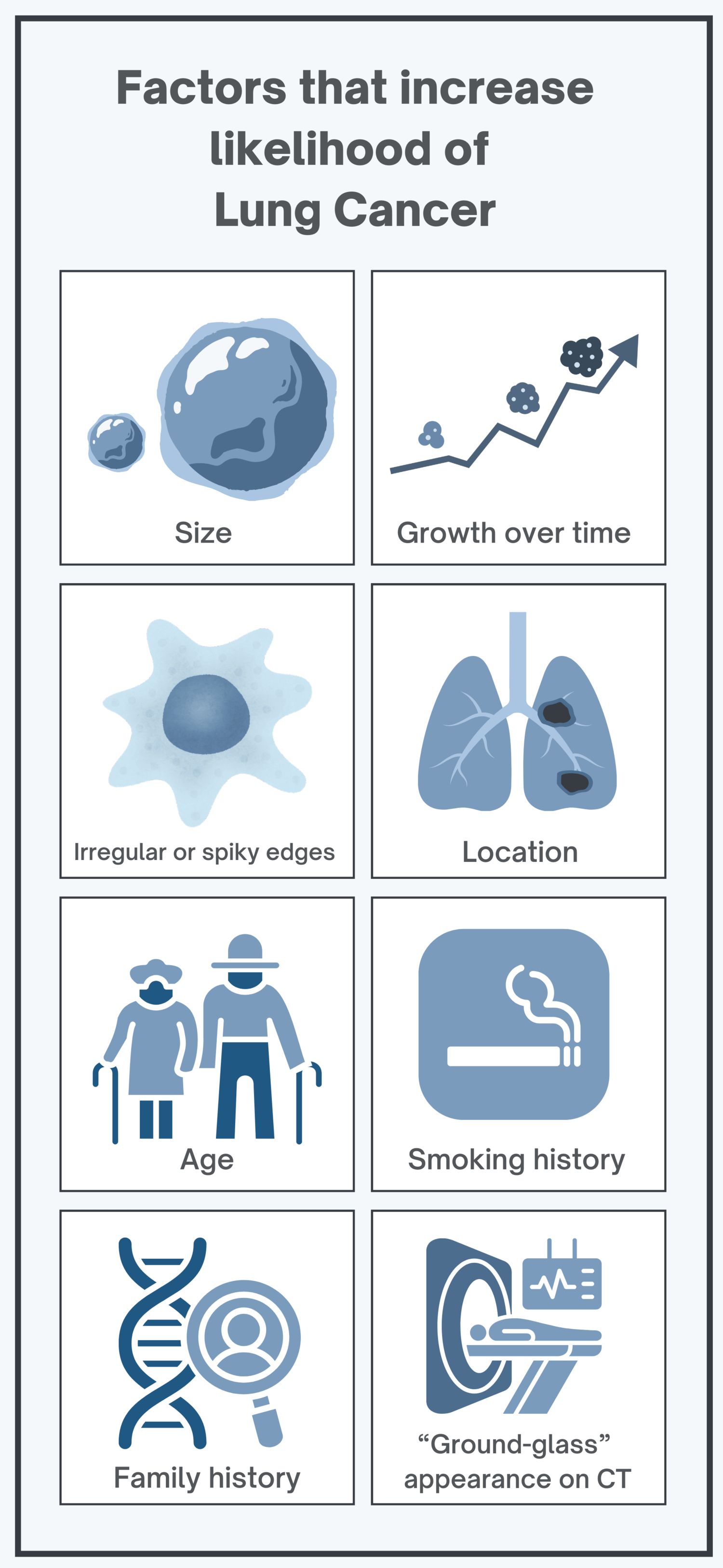
Things that tend to increase concern include:
-
Size (bigger nodules are more worrying)
-
Growth over time on repeat scans
-
Irregular or spiky edges
-
Location (some upper-lung nodules raise more suspicion)
-
Age, especially over 50
-
Smoking history
-
Family history and certain exposures (including radon, depending on circumstances)
-
“Ground-glass” or part-solid appearance on CT, which can need closer follow-up than a simple solid nodule
None of these automatically means “cancer”. They just help us decide how closely to watch, and how quickly to move.
How do we investigate a lung nodule?
We usually follow a step-by-step pathway, guided by UK practice (often BTS and NICE-aligned). The aim is to be thorough without putting you through unnecessary procedures.
Typical steps include:
-
CT scan (often low-dose): to assess the nodule’s size, shape, and exact position
-
Risk calculation tools: to estimate the likelihood of cancer and guide the next step
-
PET-CT scan (in some cases): cancers often show higher activity, which can help with decision-making
-
Follow-up imaging: many nodules are managed safely with repeat scans to check for change
-
Liquid biopsy (in selected situations): a blood test looking for tumour DNA, which can sometimes support decision-making, but it does not replace tissue biopsy when we need a definite diagnosis
-
Biopsy (only when needed): sometimes with CT guidance, sometimes via bronchoscopy, depending on location and risk
And yes, waiting for results can be the hardest part. If we are doing surveillance, it is not because we are ignoring it. It is because, for many nodules, time and imaging give the clearest answer.
“Should I worry?”
To be honest, worry is hard to switch off. But most nodules, especially small, smooth nodules in lower-risk people, are watched and prove stable.
We worry more when:
-
A nodule changes on follow-up
-
It has suspicious features on CT
-
The overall risk profile is higher (for example heavy smoking history or underlying emphysema)
The goal is not to overreact. It is to act proportionately.
Treatment options (if anything needs doing)
If the nodule is felt to be benign or low risk, the usual “treatment” is no treatment, just monitoring with repeat CT scans until we are confident it is stable
If cancer is confirmed or strongly suspected:
-
Surgery may be an option for early-stage disease (often minimally invasive in suitable cases)
-
Radiotherapy can be used in various settings, including highly targeted approaches for selected patients
-
Systemic treatments may include targeted therapy, immunotherapy, and chemotherapy, depending on the cancer type and stage
The best outcomes tend to come from finding and dealing with things early, which is why follow-up matters.
Prevention and sensible next steps
You cannot prevent every nodule. But you can reduce avoidable risk:
-
If you smoke, stopping is the single biggest step for lung health
-
Consider radon testing if relevant to where you live
-
Look after chronic lung conditions and get prompt treatment for infections
If a nodule has been found:
-
Book the follow-up appointment you have been advised
-
Ask what your estimated risk is and what guideline pathway is being followed
-
Share a proper history (smoking pack-years, occupational exposures, previous infections, travel, family history)
If you are unsure, it is reasonable to ask for a second opinion. It is your lung. You get to understand the plan.
When should you seek help?
Speak to your GP or treating team promptly if:
-
You have been told a nodule was seen and you do not have a clear follow-up plan
-
You develop symptoms such as a persistent cough, breathlessness, coughing up blood, unexplained weight loss, or ongoing chest pain
-
You have higher-risk features (age, smoking history, significant exposures) and feel you are being left in limbo
About Dr James Wilson
Dr James Wilson is a consultant oncologist specialising in lung cancer and advanced radiotherapy. Based in Central London, he works full-time in private practice, aiming to provide rapid diagnosis, clear plans, and calm, practical guidance when time matters.