How Successful Is Lung Cancer Treatment? Real Patient Stories & Options
Lung cancer treatment has been transformed by innovations like stereotactic radiotherapy, immunotherapy, and targeted therapy. In this post, Dr James Wilson shares real-life success stories from his clinic and explains how treatment is now more effective, personalised, and focused on cure, control, and quality of life.


Jump to:
- Stereotactic radiotherapy: A non-invasive alternative for early-stage lung cancer
- Neoadjuvant chemoimmunotherapy: A new standard for resectable lung cancer
- The journey of a patient with EGFR-mutated non-small cell lung cancer (NSCLC), who developed brain metastases
- Metastatic lung cancer: Extending life with better quality
- So, what does success in lung cancer look like?
Lung cancer has long been one of the most challenging cancers to treat, but thanks to medical advancements, success stories are becoming increasingly common.
I have witnessed firsthand how successful cancer research has been over the years. It has allowed many advancements and innovations to treatment options, and more importantly, it’s transformed patient outcomes. As an oncologist, there is nothing more satisfying than giving good news to a patient. Telling them their cancer is cured, or under control, is one of the greatest privileges I have.
Innovative treatments such as stereotactic radiotherapy, immunotherapy, and targeted therapies are vastly transforming patient outcomes.
So, what does successful treatment for lung cancer look like? As you can probably imagine, success is very different patient-to-patient. Where one patient’s idea of success is a cure, another person’s success is treatment that makes them feel more comfortable, and stops their cancer from growing.
Over the years, I’m really proud of the success stories I’ve seen in my clinic.
Stereotactic radiotherapy: A non-invasive alternative for early-stage lung cancer
A particularly inspiring case of mine, is that of an 84-year old man who had been diagnosed with early-stage lung cancer in the right lower lobe. Due to underlying heart conditions, surgery posed too great a risk, making him an ideal candidate for stereotactic ablative radiotherapy (SABR).
In the below photo, I’ve circled where the cancer was present in the patient. This was a tumour that, if left for a long period of time, could have caused significant damage to the patient’s lungs. Thankfully, early detection and a speedy treatment plan gave him a positive outcome.
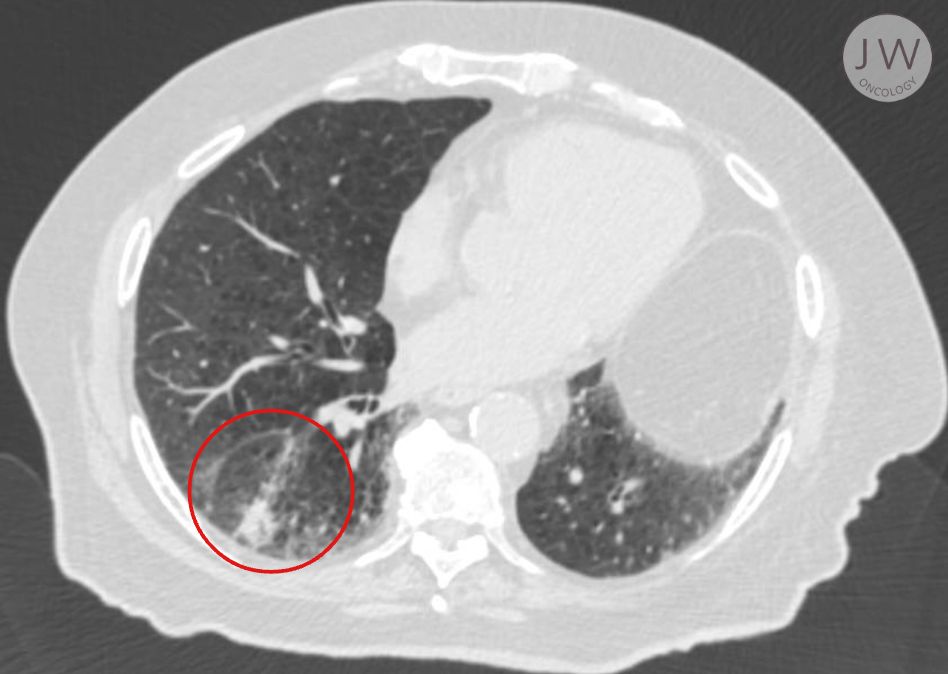
Treatment Plan: Five short treatment sessions on alternate days
Side Effects: Mild fatigue but otherwise well tolerated
Outcome: One year after treatment, imaging showed no evidence of cancer, only fibrosis and scarring.
In the image below, you can see that the area surrounding the tumour has changed drastically.
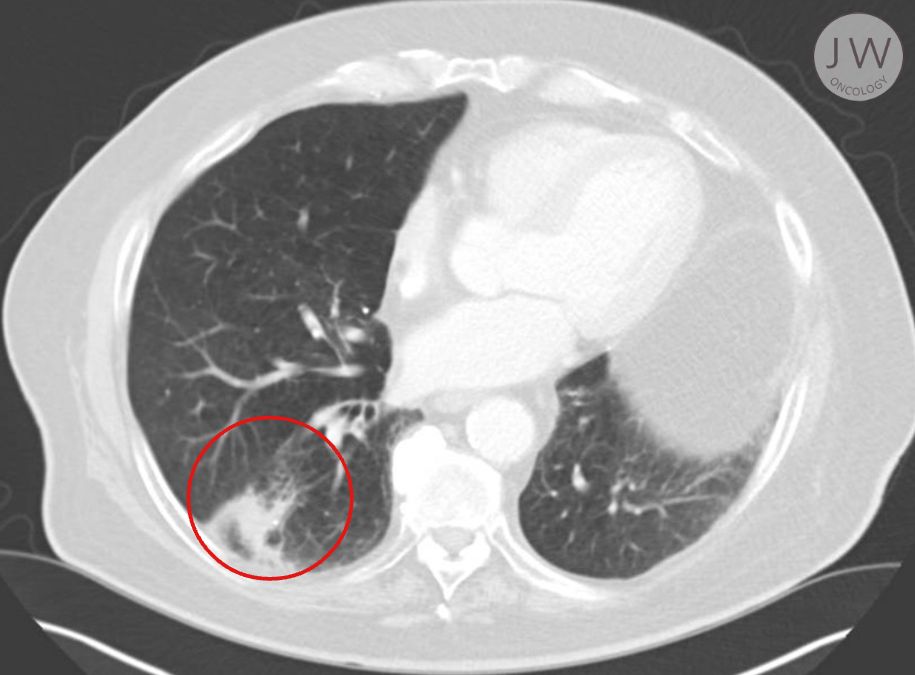
To the untrained eye, the post-treatment scan might appear concerning, but in reality, it demonstrates the power of radiotherapy. The remaining lighter matter in the x-ray is scarring and the area is cancer-free. The patient avoided invasive surgery while still achieving a high likelihood of cure. He has gone on to live a much healthier life.
Neoadjuvant chemoimmunotherapy: A new standard for resectable lung cancer
In patients who are fit for surgery, neoadjuvant (pre-surgical) treatment has revolutionised outcomes when used in carefully selected patients. One success story with a patient of mine involved a previously healthy patient with a tumour in the right upper lobe of his lung. This patient received chemoimmunotherapy before surgery, allowing the immune system to better recognise and attack the tumour.
Circled in the below image, you can see this patient’s tumour was significant in size in the right lung (left of the image) and would very much benefit from surgery.
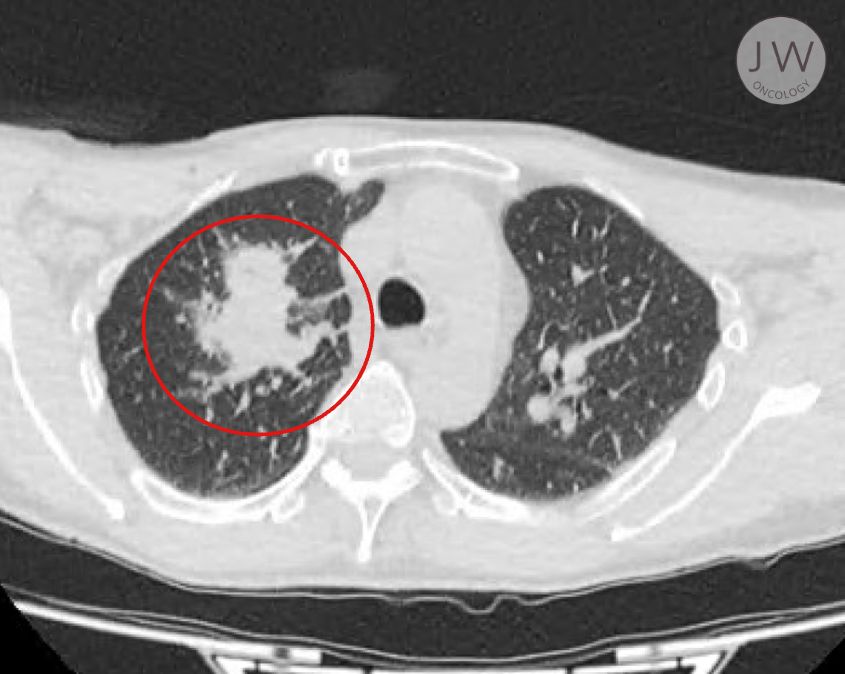
Treatment Plan: Chemotherapy and immunotherapy before surgery
Surgical Outcome: The affected lung lobe was removed
Pathology Results: No remaining cancer, only evidence of white blood cells and fibrosis
This case highlights how neoadjuvant treatment enhances the curability of lung cancer. Rather than relying solely on chemotherapy post-surgery, this approach maximises the immune system’s ability to fight cancer before it spreads.

In the image above, you’ll see the significant difference that surgery and chemotherapy and immunotherapy had in this case. Again, this was concluded as a cure, and the patient now leads a healthy life with checks now and again over the next every five years.
The below image is of the lung tissue after it was removed and looked at under the microscope. As a result of the chemoimmunotherapy, there was no cancer left. The immunotherapy has stopped the cancer hiding from this patient’s immune system (cancer has a tendency to be able to stop the white blood cells doing their job, allowing the cancer to spread).
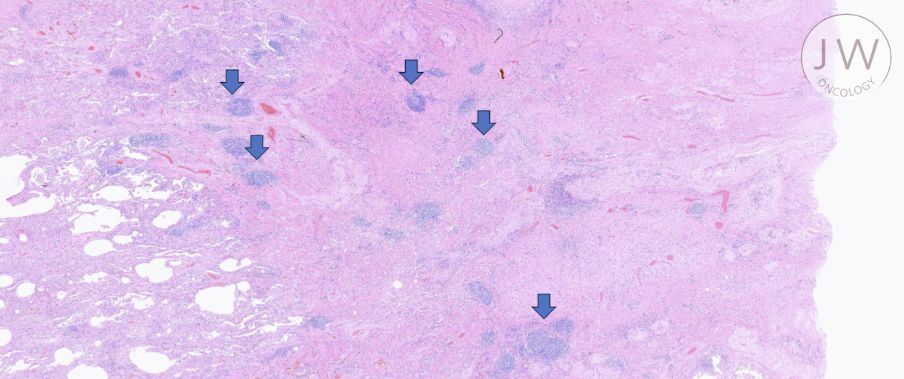
This particular case is an excellent example of cancer research being used in real-time. Where we used to perform surgery first, and then administer chemotherapy and immunotherapy afterwards, there have been far more success stories where immunotherapy and chemotherapy have been able to prevent the cancer cells from developing pre-surgery as opposed to afterwards.
The journey of a patient with EGFR-mutated non-small cell lung cancer (NSCLC), who developed brain metastases
Lung cancer treatment has seen remarkable advancements, offering new hope to patients with metastatic disease. This case highlights the journey of a patient with EGFR-mutated non-small cell lung cancer (NSCLC), who developed brain metastases but responded exceptionally well to targeted therapy and stereotactic radiosurgery.
The patient, diagnosed with EGFR-mutant NSCLC, initially responded well to treatment. However, disease progression led to the development of brain metastases.
To target the brain metastases, the patient underwent CyberKnife stereotactic radiosurgery, a highly precise radiation technique minimising damage to surrounding brain tissue.
The combination of targeted therapy and CyberKnife led to remarkable disease control. Follow-up scans (seen in the below images) showed significant reduction in intracranial disease burden, with the patient maintaining excellent neurological function and quality of life. He also remained on the first-line treatment for his lung cancer for a long time after this treatment - delaying the time until he needed to have chemotherapy.
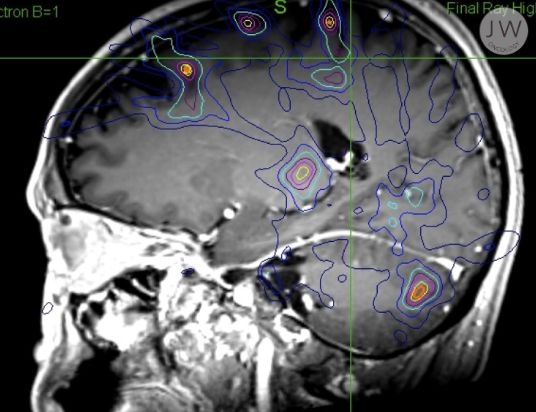
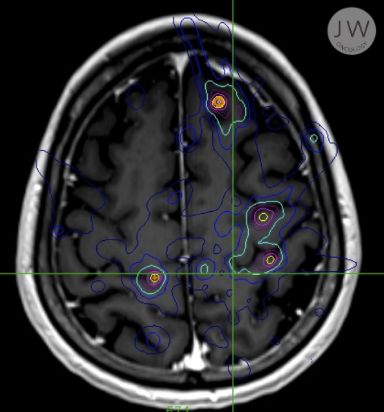
Treatment Plan: Prevent further spread of disease with TKI and CyberKnife stereotactic radiosurgery
Outcome: Remarkable disease control
Pathology Results: Significant reduction in intracranial disease burden. This case is a testament to the power of multimodal therapy, providing patients with better outcomes and extended survival.
Metastatic lung cancer: Extending life with better quality
For patients with metastatic lung cancer, the goal is to extend a patient’s life while maintaining comfort and quality. One of the biggest wins in oncology is the ability to control cancer in multiple locations using targeted therapies and stereotactic radiation.
Key benefits include:
-
Non-invasive treatments with minimal side effects
-
The ability to “zap” cancer when it spreads to new areas
-
Prolonged survival, even when cancer is not curable
With emerging options like DATAR testing, which analyses the genetic signature of cancer, we can personalise treatment even further, opening the door to cutting-edge drugs and therapies not yet widely available on the NHS.
So, what does success in lung cancer look like?
For early-stage cancer: Quick, effective treatment before the disease spreads
For metastatic cancer: Prolonged survival with minimal disruption to daily life
For all patients: Maximising time, comfort, and treatment effectiveness
The landscape of lung cancer treatment is changing dramatically. Whether through stereotactic radiotherapy, neoadjuvant therapies, or targeted treatments, we are seeing more patients live longer, fuller lives. While we may not always achieve a cure, we are increasingly able to control cancer, minimise suffering, and offer real hope.
Lung cancer is no longer an immediate death sentence. With the right treatments, patients are living longer, feeling better, and experiencing true success in their cancer journey.
I’m passionate about helping you find the best option for whatever you’re currently facing. For me, putting your cancer journey in my hands is a privilege I don’t take lightly. I aim to offer you the best results possible for yourself and your loved ones and understand the stress you are facing when choosing an oncologist.
If you’d like to chat through your current diagnosis to get an idea what I can offer, then please do get in touch.
Visit here to schedule an appointment or give me a call at +44(0)20 7993 6716
Here's a link to my video, discussing what success in lung cancer treatment may look like, and the three examples in more detail.
How Successful Is Lung Cancer Treatment? — Dr. James Wilson (an Oncologist in the UK)