Thymoma Treatment: Expert Care in London
Discover expert care for thymoma in London with Dr James Wilson. Learn about diagnosis, treatment options, and personalised support for this rare tumour. Book your consultation today.


In the News: Dr Wilson talking about thymoma on ITV’s This Morning
When opera singer Lesley Garrett faced a complex cancer diagnosis, she turned to Dr James Wilson for fast, personalised care. Her story was featured in the Mail on Sunday and on This Morning.

Watch the video below:
When patients are told they may have a rare tumour like thymoma, many feel overwhelmed. The diagnosis can be uncertain, and standard pathways may not always offer fast answers or specialist input. That’s where a personalised, joined-up approach really matters.
As a consultant oncologist in full-time private practice, I regularly see patients with thymoma, often with linked conditions such as myasthenia gravis. My role is to help them get clarity quickly, coordinate the right experts, and guide them through treatment choices with confidence.
You're welcome to request a consultation if you’d like to talk through a diagnosis or get a tailored opinion.
What is Thymoma?
Thymoma is a rare cancer that develops in the thymus gland, a small organ located in the upper chest behind the breastbone. The thymus gland plays a crucial role in your immune system, particularly during childhood development. As a rare tumour, thymoma requires specialised expertise for proper diagnosis and treatment.
Thymomas are distinct from other cancer types in several important ways. Unlike many aggressive cancers, thymomas typically grow slowly and don't often spread widely throughout the body. However, they can be invasive, growing into nearby structures within the chest. Lymph node involvment is rare. Many patients with thymoma also experience autoimmune disorders, most notably myasthenia gravis, which affects approximately 30-40% of thymoma patients.
Though sometimes referred to as "benign thymoma," this terminology is misleading. All thymomas have malignant potential and are considered a form of thymus gland cancer. The World Health Organisation (WHO) classifies thymomas into different types (A, AB, B1, B2, B3) and thymic carcinoma, based on the appearance of the cancer cells and the proportion of lymphocytes (white blood cells) present. This classification guides treatment decisions and helps predict outcomes.
Types of Thymic Tumours
Thymic epithelial tumours include thymomas and thymic carcinomas. Understanding the specific type is essential for determining the best treatment approach:
Types of Thymoma
Based on the World Health Organisation classification, thymomas are categorised by how the cancer cells look under a microscope:
-
Type A Thymoma: Comprised mainly of spindle or oval-shaped epithelial cells with few lymphocytes. These typically have an excellent prognosis.
-
Type AB Thymoma: Contains a mixture of type A cells and areas rich in lymphocytes. This is the most common type and generally has a favourable outlook.
-
Type B1 Thymoma: Resembles normal thymic tissue with abundant lymphocytes. Generally has a good prognosis.
-
Type B2 Thymoma: Contains more epithelial cells than B1, though lymphocytes remain abundant. More likely to be invasive than types A, AB, and B1.
-
Type B3 Thymoma: Predominantly epithelial cells with few lymphocytes. These are more aggressive with a higher risk of recurrence.
Thymic Carcinoma
Thymic carcinoma is a more aggressive of thymic tumour (sometimes called thymus cancer or malignant thymoma) with clear cancerous features. It behaves more aggressively than the thymoma cancer type, growing quickly and often spreading to other parts of the body. Treatment typically requires a more intensive approach and use of a different treatment option.
Collectively, thymomas and thymic carcinomas are known as thymic epithelial tumours, representing the most common tumours of the anterior mediastinum (the front part of the chest between the lungs).
Symptoms of thymoma and Diagnosis
Common Symptoms of thymoma
Many patients with thymoma have no symptoms at all, with the tumour discovered during tests for other conditions. When symptoms do occur, they may be quite vague, but include:
-
Chest pain
-
Persistent cough
-
Difficulty breathing or shortness of breath
-
Swelling in the face and neck
-
Muscle weakness (particularly if myasthenia gravis is present)
-
Unexplained weight loss or fatigue
Around 30-40% of thymoma patients develop myasthenia gravis, an autoimmune condition causing muscle weakness, particularly affecting the eyes, face, throat, and limbs. Less commonly, thymoma can be associated with other conditions like pure red cell aplasia or hypogammaglobulinemia.
Diagnostic Process
If a thymoma or thymic cancer is suspected, your doctor will likely recommend:
-
CT scan: The primary imaging method for suspected thymoma, providing detailed information about the tumour's size, location, and potential invasion
-
MRI: Sometimes used to complement CT, particularly to distinguish thymic tumours from other masses
-
FDG-PET/CT: I will discuss whether we need to do a PET scan with you based on your personal situation
-
Blood tests: Including tests for autoantibodies associated with myasthenia gravis, and other blood tests to rule out other conditions which can look like thymoma on scans (e.g. germ cell tumours)
-
Biopsy: In some cases, tissue sampling may be necessary to confirm the diagnosis
Early and accurate diagnosis is crucial for developing an effective treatment plan. As a specialist in thymic malignancies, I ensure a thorough diagnostic process that guides personalised treatment recommendations.
Treatment Option Overview for Thymoma and Thymic Carcinoma
Treatment for thymoma and thymic carcinoma is highly individualised, based on the type and stage of the tumour, your overall health, and the presence of associated conditions like myasthenia gravis. As a thymic cancer specialist, I offer comprehensive treatment using the latest evidence-based approaches.
Surgery
Surgical removal remains the cornerstone of treatment for thymoma whenever possible. Complete removal of the tumour, including the entire thymus gland (thymectomy), offers the best chance for cure, particularly for early-stage disease.
Modern surgical approaches include:
-
Traditional open surgery: Via an incision through the breastbone
-
Minimally invasive techniques: Including video-assisted thoracoscopic surgery (VATS) and robotic-assisted approaches for suitable patients
-
Extended resection: For invasive thymoma, may include removal of affected surrounding structures
The goal is complete removal of the tumour with clear margins. The completeness of resection significantly influences long-term outcomes.
Radiation Therapy
Radiation therapy plays several important roles, and is considered standard treatment, in the management of thymic tumours:
Post-operative (Adjuvant) Radiation Therapy
For many patients, especially those with more advanced disease or aggressive tumour types, radiation therapy after surgery helps reduce the risk of recurrence. As a specialist in thymic malignancies,and a clinical oncologist (sometimes referred to as radiation oncologists) to determine if this is the best treatment approach for you.
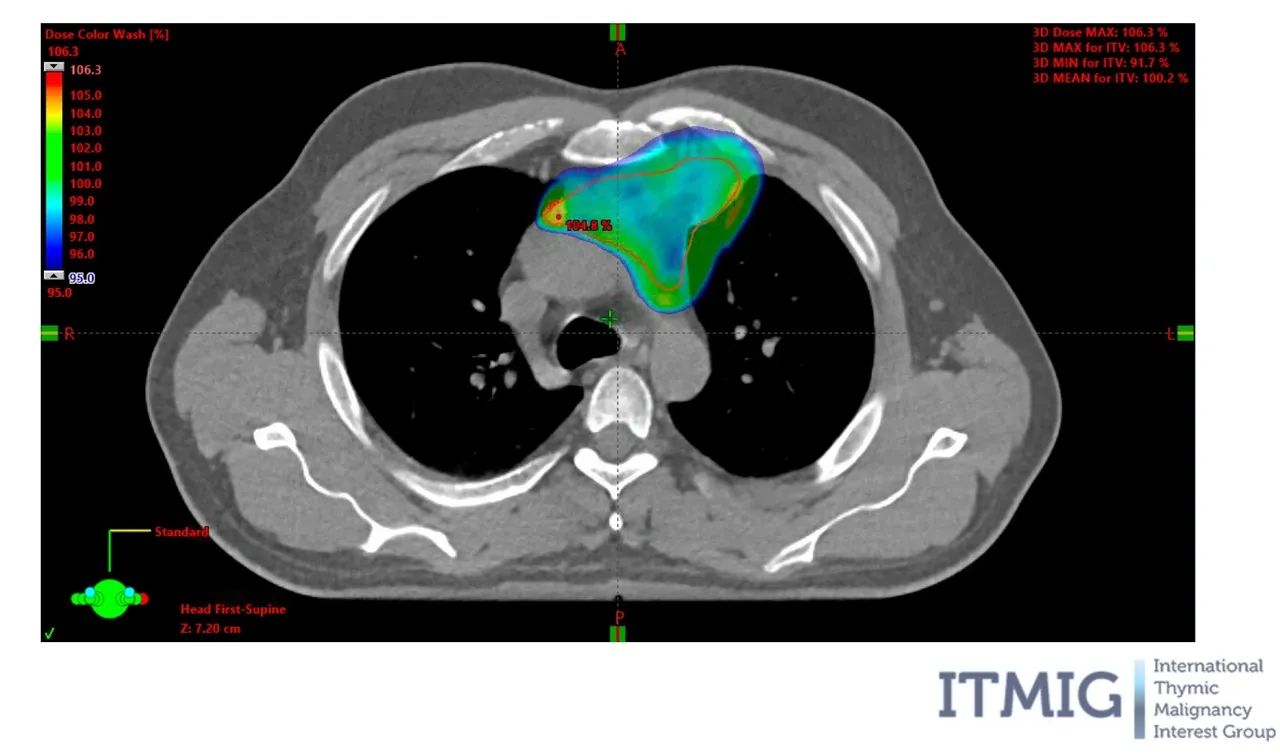
Modern radiation techniques allow for precise targeting of the tumour bed while minimising exposure to surrounding healthy tissues like the heart and lungs. I am able to offer proton beam therapy for thymoma.
Definitive Radiation Therapy
When surgery isn't possible, radiation therapy may be the primary treatment approach, often combined with chemotherapy. Advanced techniques like intensity-modulated radiation therapy (IMRT) allow for effective treatment with reduced side effects.
Chemotherapy
Chemotherapy may be recommended in several scenarios:
-
Before surgery (neoadjuvant chemotherapy) to shrink large or invasive tumours
-
After surgery (adjuvant chemotherapy) for high-risk or incompletely removed tumours
-
As primary treatment for advanced or metastatic disease (stage IV thymoma)
-
In combination with radiation therapy (chemoradiation)
-
As a treatment for recurrent thymoma
Common chemotherapy regimens for thymic tumours include cisplatin-based combinations. The specific protocol is tailored to your individual situation and tumour characteristics. For example different chemotherapy is used in combination with radiotherapy than in stage IV thymoma.
Targeted Therapy and Immunotherapy
For advanced or recurrent disease, newer treatment approaches may include:
-
Targeted therapy: Drugs that target specific molecular changes in cancer cells
-
Immunotherapy: Treatments that help your immune system recognise and attack cancer cells - it is used more for thymic carcinoma as it doesn't seem to be of benefit as a treatment for thymoma
These approaches are continually evolving, with ongoing clinical trials evaluating new options for patients with thymic malignancies. I am always happy to discuss yout clinical trial options with you.
Specialised Treatment for Different Stages
Early-Stage Thymoma
For stage 1 and stage 2 thymoma, surgery alone may be sufficient, though radiation therapy would be considered standard treatment if the thymic tumour has certain high-risk features. The 5-year survival rates for early-stage disease typically exceed 80%.
Locally Advanced Thymoma
Stage III and IVA disease (where the cancer has spread locally but not to distant sites) often requires multimodal treatment with surgery, radiation therapy, and sometimes chemotherapy. Even with locally advanced disease, long-term disease control is often achievable.
Metastatic or Recurrent Disease
For stage IVB or recurrent thymoma, treatment options include:
-
Surgery for isolated or limited metastases
-
Radiation therapy for local control, including stereotactic radiotherapy to eliminate the recurrence
-
Systemic therapy (chemotherapy, targeted therapy, or participation in clinical trials)
-
Combination approaches
Even with advanced thymoma, many patients can achieve prolonged disease control and good quality of life with appropriate treatment.
The Importance of Specialist Care for Thymic Tumours
As rare cancers, thymomas and thymic carcinomas benefit tremendously from specialist care. The complexity of these tumours requires expertise in:
-
Accurate interpretation of imaging and pathology
-
Surgical techniques specific to the mediastinal region
-
Appropriate use of radiation therapy and systemic treatments
-
Management of associated autoimmune conditions
-
Access to clinical trials and innovative approaches
As a specialist clinical and radiation oncologist focused on thymic malignancies, I offer:
-
Extensive experience in the management of these rare tumours
-
A multidisciplinary approach, collaborating with expert thoracic surgeons, radiation oncologists, and other specialists
-
Access to the latest treatment modalities and clinical trials
-
Personalised care plans that consider your unique situation
It is important that you see a doctor who sees lots of patients each year with thymoma to ensure you get the best treatment.
Post-operative Radiotherapy following thymectomy
Post-operative radiotherapy represents a critical component in the management of thymoma for many patients. The decision to recommend radiotherapy after surgery involves careful consideration of several factors, including the stage of the disease, completeness of surgical resection, histological subtype, and individual patient characteristics.
When is Post-operative Radiotherapy Recommended?
Current evidence and clinical guidelines suggest:
-
Stage I thymomas: Post-operative radiotherapy is generally not indicated after complete resection, as the risk of recurrence is very low.
-
Stage II thymomas: The recommendation depends on the histological subtype and the extent of invasion:
-
For less aggressive types with complete resection: Radiotherapy may be omitted
-
For more aggressive types (B2 and B3): Radiation therapy is often recommended due to higher recurrence risk
-
For any incompletely resected tumour: Radiotherapy is strongly recommended
-
-
Stage III/IVA thymomas: Post-operative radiotherapy is generally recommended for all patients, regardless of histology or completeness of resection, due to the high risk of local recurrence.
-
Thymic carcinoma: Recurrent thymic carcinoma can be challenging to treat, so taking measures to prevent it coming back are usually recommended. Futher treatment with either chemotherapy, radiotherapy or a combination (chemoradiotherapy for thymic cancer) is generally offered after surgery to reduce the risk of the thymus cancer coming back.
Modern Radiotherapy Techniques
Delivery of post-operative radiotherapy for thymoma requires expertise and precision:
-
Intensity-modulated radiation therapy (IMRT) allow for precise targeting while minimising exposure to critical structures
-
I am able to offer proton beam therapy (PBT) to patients with thymoma to minimise the risk of long-term side effects
These advanced techniques help maximise tumour control while minimising side effects, potentially improving both outcomes and quality of life during and after treatment.
Clinical Trials and Research
Ongoing clinical trials are evaluating new approaches for thymic tumours, including:
-
Novel chemotherapy combinations
-
Targeted therapies based on molecular profiling
-
Immunotherapy strategies
-
New radiation techniques
As a specialist in thymic malignancies, I stay current with the latest research and can help determine if participation in a clinical trial might be appropriate as part of your treatment plan.
The National Cancer Institute and major cancer centres around the world, including leading institutions in the UK, continue to advance our understanding of these rare tumours and develop more effective treatments.
Living with Thymoma
A thymoma diagnosis affects not just your physical health but every aspect of your life. Comprehensive cancer care includes:
-
Managing treatment side effects
-
Monitoring for recurrence
-
Addressing associated conditions like myasthenia gravis and other autoimmune conditions
-
Supporting your emotional wellbeing
Many thymoma patients lead full and active lives during and after treatment. With appropriate care, the prognosis for thymoma is often more favourable than for many other cancer types.
Frequently Asked Questions
Is thymoma a type of cancer?
Yes, thymoma is considered a type of cancer that originates in the thymus gland. However, it differs from many other cancers in several important ways. Thymomas typically grow more slowly, are less likely to spread widely throughout the body, and generally have a better prognosis than many other malignancies.
All thymomas have malignant potential, meaning they can invade surrounding structures and, in some cases, spread to distant sites. The WHO classification and staging system provide more accurate ways to describe the aggressiveness and extent of thymoma.
Does everybody with thymoma need radiotherapy?
No, not every patient with thymoma requires radiation therapy. The need for radiotherapy depends on several factors, including the stage of the disease, the completeness of surgical resection, and the histological subtype of the thymoma.
For completely resected stage I thymomas, radiotherapy is generally not recommended. For stage II thymomas, the decision depends on the tumour type and extent of invasion. For stage III and IVA thymomas, post-operative radiotherapy is typically recommended due to the higher risk of recurrence.
Each case should be discussed with a specialist to determine the optimal treatment approach based on individual characteristics and the latest evidence.
What is the relationship between thymoma and myasthenia gravis?
Thymoma and myasthenia gravis share a remarkable association, with approximately 30-40% of thymoma patients developing myasthenia gravis. Conversely, about 10-15% of patients with myasthenia gravis will have a thymoma.
Myasthenia gravis is an autoimmune disorder causing muscle weakness, particularly affecting the eyes, face, throat, and limbs. In thymoma patients, the abnormal thymic tissue may trigger the production of harmful autoantibodies.
For patients with both conditions, treating the thymoma is essential, but specific management of the myasthenia gravis (with medications such as acetylcholinesterase inhibitors and immunosuppressants) is also necessary. Close collaboration between oncologists and neurologists ensures optimal care.
What are the different types of thymoma and how do they affect treatment?
Thymomas are classified according to the World Health Organisation (WHO) system into types A, AB, B1, B2, B3, and thymic carcinoma, based on the appearance of the cancer cells and the proportion of lymphocytes present.
Types A and AB are generally less aggressive, while types B1, B2, and B3 form a spectrum of increasingly aggressive behaviour. Thymic carcinoma is the most aggressive type with a higher likelihood of spread.
This classification influences treatment decisions, including:
-
Surgical approach and extent
-
Whether to recommend post-operative radiation therapy
-
Need for chemotherapy or other systemic treatments
The WHO classification, along with staging, forms the foundation for personalised treatment planning.
What are the treatment options for recurrent thymoma?
When thymoma recurs after initial treatment, several options may be considered:
-
Surgery: If the recurrence is localised and technically resectable
-
Radiation therapy: Particularly if not used previously or for small, well-defined recurrences
-
Systemic therapy: Chemotherapy or targeted agents for widespread recurrence
-
Clinical trials: Investigating novel therapies
Many patients with recurrent thymoma can achieve meaningful disease control, sometimes for many years, through one or more of these approaches. The prognosis for recurrent disease is generally more favourable than for many other recurrent cancers.
Thymoma Treatment London: Expert Care in the UK
As a clinical oncology specialist in the treatment of thymic tumours, I provide comprehensive care for people with thymoma and thymic carcinoma at leading hospitals in London. With specialist thymoma expertise in both standard treatments and cutting-edge approaches, I work closely with a multidisciplinary team to ensure each patient receives optimum care.
UK-Wide and International Patient Care
Please do not feel constrained by the location of my practices in London; many of my patients live outside the capital and the UK. To accommodate those coming from afar, I offer initial video consultations to promptly develop personalised care and treatment plans that meet your needs and can be implemented quickly.
For patients requiring thymoma treatment in London who live elsewhere in the UK or internationally, my team can provide guidance on practical considerations for your stay in London. The UK is recognised globally for excellence in thymoma care, with London hosting world-class facilities and the latest treatment modalities for thymic epithelial malignancies. People travel from all over the world for cancer treatment at the London hospitals where I see thymoma patients.
Why Choose Specialist Care?
For rare cancers like thymoma and thymic carcinoma, specialist expertise significantly impacts outcomes. Benefits of specialist care include:
-
Accurate diagnosis and staging: Crucial for developing the optimal treatment plan
-
Surgical expertise: Technical skill in complete resection of the tumour
-
Appropriate use of additional therapies: Making evidence-based decisions about radiation therapy, chemotherapy, and newer treatment approaches
-
Management of associated conditions: Including myasthenia gravis and other autoimmune disorders
-
Access to clinical trials: Potential opportunities to receive innovative treatments
My practice combines medical expertise with a patient-centred approach, ensuring you receive not just the most advanced care, but also support and guidance throughout your treatment journey.
To schedule a consultation, please get in touch. Virtual consultations are available for thymoma patients throughout the UK and internationally, ensuring that geography is not a barrier to accessing expert care for thymoma.
Take the next step towards expert thymoma treatment by reaching out today.
Take Control of Your Thymoma Treatment with Dr James Wilson
Facing a diagnosis with a rare cancer such as thymoma requires expert guidance and cutting-edge treatment. My specialist interest in thymoma, advanced chemoradiotherapy techniques, combined with access to the latest technologies, provides you with the best possible chance of successful treatment.
Every patient's journey is unique, and I'm committed to providing personalised care that addresses your specific needs and circumstances. From initial consultation through treatment completion and beyond, I'll be your dedicated partner for thymoma treatment and follow-up.
The combination of my expertise, advanced technology, and comprehensive support team creates an environment where you can focus on healing while receiving world-class care. Together, we'll develop a treatment plan that maximises your chances of cure while maintaining your quality of life.
Don't delay in seeking expert care. Early treatment provides the best outcomes, and every day matters in cancer care.
Call +44 (0)20 7993 6716 or email us to schedule a consultation and explore chemoradiotherapy options tailored to you.
Take the first step towards expert cancer care today. Contact us to arrange your consultation and begin your journey towards the best possible treatment outcome.
Book your appointment directly by clicking here.