Dr James Wilson | London Lung & Skin Cancer Specialist
Rapid, consultant-led cancer treatment without NHS delays. I work with you and your family to get you the best cancer treatment as quickly as possible.
If you or someone you love has just been diagnosed with lung cancer or skin cancer, or you need strategic radiotherapy for Stage 4 cancer, I can help you understand your options and start treatment fast.
Consultant oncologist specialising in lung cancer, melanoma and skin cancer. From curative treatment for early-stage disease to strategic care for advanced cancer.
Offering private cancer treatment to patients across the UK and international patients seeking expert care in London. Private health insurance accepted, and transparent self-pay options available.
-
Know your cancer treatment options within days, not months
-
Private consultations usually available within 48 hours - without long delays or confusing pathways
-
Request an appointment and we'll guide you through the rest. Let us be your cancer expert so you don't have to be

As featured in...


Stage 4 Cancer: SABR Treatment
Highly targeted radiotherapy. Fewer side effects. More time for life.
Could SABR help me?Meet Dr James Wilson – Your Private Oncology Consultant in London
University of Oxford, Royal Marsden Hospital and Massachusetts General Hospital trained | Former UCLH consultant | One of the UK's few specialists offering both advanced drug therapies and precision radiotherapy including proton beam therapy and SABR
Book nowExpert Private Cancer Treatment in London: Better Options, Faster Access
✓ Appointments on the same or next day
Because time matters
✓ No GP referral required
We work alongside your NHS care if needed
✓ Fast-track video consultations
Find out how we can help
✓ Early treatment
Can make all the difference - cancer doesn't wait
Feeling Lost in the System? Wondering if there are better cancer treatment options? You're in the right place if:
You've been diagnosed with lung cancer, melanoma or skin cancer
Whether you need a personalised treatment plan for early-stage disease or strategic care for advanced cancer, I provide comprehensive clinical care tailored to your individual needs. My service includes coordinating all scans, biopsies, and support from nurses and specialists throughout your journey - all delivered within days, not weeks.
You have cancer that has spread to just a few sites (oligometastatic disease)
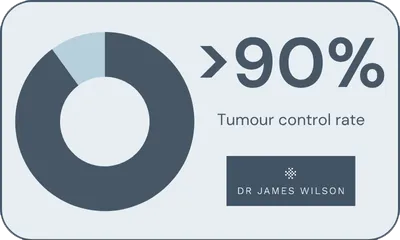
When cancer has spread to 1-5 specific locations, you have more options than you might think. SABR (stereotactic radiotherapy) can precisely target these spots with remarkable success rates—over 90% tumour control for treated areas. This applies to any cancer type: lung, breast, prostate, colorectal, melanoma and others.
Your cancer treatment is working - except in one or two spots (oligoprogressive disease)
If most of your cancer is controlled but one or two areas are growing, you don't need to abandon a working treatment. SABR can target those problem spots while you continue your current therapy, keeping you on effective treatment longer and saving other options for when you truly need them.
You've been offered palliative care only
If you've been told there are no active treatment options for your cancer, it's worth exploring whether SABR, advanced immunotherapy, proton beam therapy or targeted therapies could offer a different path forward. Not all oncologists have access to these treatments or specialise in them.
You're frustrated with NHS delays and want rapid access to treatment
Time matters with cancer. I can arrange all necessary scans, molecular profiling and treatment within days—not months. You won't lose your NHS care by seeking private treatment for specific aspects of your care. All your records are shared seamlessly so your care remains joined up.
Private Cancer Treatment London: What Patients Say About Dr James Wilson
The fact that James was prepared to go the extra mile, and he was on holiday when I called, speaks volumes for him. Honestly, if I didn't think he was as good as he is, I wouldn't be sitting here now talking to you."
- Patient testimonial
When you're facing a cancer diagnosis, you need more than medical expertise—you need a doctor who treats you as a person, not just a patient.
Book nowWhat Sets Private Cancer Treatment with London Oncologist Dr James Wilson Apart?
✓ A consultant who answers the phone
Your questions can't wait weeks for an appointment. Whether you're experiencing side effects from immunotherapy, worried about scan results, or simply need reassurance, you'll get same-day responses. No waiting for callbacks. No being passed between junior doctors who don't know your case.
✓ Treatment decisions made together
You'll never be told "this is your only option" without understanding why. Every lung cancer treatment plan, melanoma therapy choice, or SABR radiotherapy recommendation is explained in plain English. You're an equal partner in every decision, with time to ask questions until you truly understand.
✓ One consultant throughout your entire journey
From your first consultation through treatment and follow-up, you see the same consultant at every appointment. Our dedicated nurses also provide continuous support, ensuring you have the information and care you need at every stage. No handoffs to junior doctors. No repeating your history to strangers. Just continuity, trust, and people who know your case intimately.
✓ Fast access when time matters most
The period between diagnosis and starting treatment is agonising. Why spend it waiting? Get scans within 48 hours, molecular profiling within a week, and treatment started immediately. Private oncology in London means your timeline is driven by medical necessity, not system capacity.
What happens next. From cancer diagnosis to treatment in 3 simple steps

Step 1: Book a Consultation
Speak to our specialist team. No referral needed. We'll review your case and schedule your appointment without delay.
The earlier we act, the more choices we have.

Step 2: Receive a Tailored Treatment Plan
Based on your scans, tests, and goals - we build a precise personalised plan, using the latest evidence-based therapies.
We’ll explain all costs upfront before any commitment. No obligation. Just answers.

Step 3: Begin Treatment Quickly
Whether it's immunotherapy, CyberKnife, or precision radiotherapy - we start without delay. We will guide you through each stage with the utmost care.
Every day counts - that’s why we help you begin treatment without unnecessary delay.
SABR Treatment Success Rates: Over 90% Cancer Control
Whether treating early-stage lung cancer with curative intent or targeting oligometastatic disease sites, stereotactic radiotherapy (SABR) achieves exceptional tumour control rates. These are my personal outcomes treating patients across London - not national averages, but real results from my practice.
My Approach to Private Cancer Care: London Clinics or Home-Based Treatment
If you or someone you love has just been diagnosed with cancer, time matters. I provide fast access to advanced cancer treatment at London’s leading private hospitals, with no unnecessary delays.
My approach combines targeted, evidence-based therapies with truly personalised care. As your consultant, I don’t just offer clinical expertise. I act as your advocate. I make sure nothing is missed, and no one is left waiting.
Many of the people who come to me are sons, daughters, or partners searching for better options for someone they love. You’re not alone. When the NHS is overwhelmed and time feels critical, private care can offer speed, clarity, and reassurance.
Treatment delivered at leading private hospitals in London or via coordinated cancer services at your local hospital, or your own home.
I care for every patient with the same urgency and dedication I would want for my own family. That means no switchboards. No long waits. Just expert care, delivered when and where it’s needed most.
Get in touch. We'll guide you through the next step.
Getting Clear Answers About Your Diagnosis, Cancer Staging and Treatment Options
Whether you've just been diagnosed with early-stage cancer or been told your cancer has spread, the most important thing right now is getting clear answers about your treatment options and starting the right plan as quickly as possible.
You have more options than you might think
Modern cancer treatment has advanced significantly. When cancer spreads to just a few sites (oligometastatic disease), targeted SABR treatment can eliminate those deposits with 90-95% control rates. For early-stage lung cancer, SABR offers cure rates comparable to surgery without an operation. For advanced melanoma, breakthrough immunotherapies are achieving responses that weren't possible five years ago.
Speed matters
Rather than waiting weeks in NHS queues while your cancer potentially progresses, you can get all necessary scans, biopsies and molecular profiling completed within days. Treatment can start within a week. And you won't lose your NHS care - I work with your existing team to coordinate everything seamlessly.
Here's what makes the difference:
Dr James Wilson, London oncologist, can offer you the full spectrum of treatment options - from curative SABR radiotherapy and proton beam therapy to breakthrough immunotherapies, targeted drugs and chemotherapy, all coordinated as one seamless plan. You're not limited to what's available at a single hospital or through one type of specialist.
Access to the right information is crucial when making cancer treatment decisions. I ensure you understand your diagnosis, all available options including clinical trials when appropriate, and what standard care looks like versus cutting-edge approaches and world-leading technology. Every treatment plan is built around your individual needs and circumstances, not a one-size-fits-all protocol.
No more delays
No more unanswered calls. No more wondering if you're getting the best possible care. You'll receive the right drug treatment for your specific cancer type, molecular profiling to identify targeted therapies, access to clinical trials when appropriate, and rapid-access scans and results, typically same or next day.
Your next step is simple:
Get a clear, personalised assessment of whether this combined approach is right for your situation. You'll have answers within 48 hours, not weeks.
Stop relying on Google for answers and seek expert advice and guidance that cares for you and removes barriers to the care that you need
Cancer Types We Treat: Lung Cancer, Melanoma & Skin Cancer in London


-
Treated Condition
Private Lung Cancer Treatment in London - Fast Access, Expert Care
Lung cancer is serious, but early detection and modern treatments offer real hope. I use advanced technologies to provide curative options, even in complex cases.
Learn more ↗ -
Treated Condition
Private Melanoma Treatment in London: Expert-Led, Fast Access Cancer Care
Melanoma is the most invasive type of skin cancer. Although it poses significant health risks, it is highly treatable when detected early and addressed proactively with targeted cancer therapy.
Learn more ↗ -
Treated Condition
Skin Cancer
Non-melanoma skin cancer is a type of skin cancer that develops in the outer layers of the skin, particularly in the basal and squamous cells. The most common types are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC).
Learn more ↗ -
Treated Condition
Metastatic Disease or Stage 4 Cancer
When cancer spreads beyond its original site, we call it 'metastatic disease' - sometimes referred to as 'Stage 4 cancer'.
Learn more ↗ -
Treated Condition
Thymoma and thymic carcinoma treatment
As a clinical oncology specialist in the treatment of thymic tumours, I provide comprehensive care for patients with thymoma and thymic carcinoma at leading hospitals in London.
Learn more ↗
Working With Your NHS Team To Get The Best Outcome For You From Your Private Cancer Treatment
But if I go private, can I still have NHS treatment?"
This is the question I hear most often - and what surprises me is the reason behind it. It's not just about practicalities. Many patients feel a sense of loyalty. They worry about offending their NHS team or losing their place in the system.
If you're a UK resident, you're entitled to NHS treatment regardless of whether you've received some investigations or care privately.
Your wellbeing comes first. Using private care for specific aspects of treatment - particularly time-sensitive interventions like SABR for oligometastatic disease - can actually enhance your overall cancer care rather than complicate it.
If you're hesitating because you feel conflicted about loyalty to the NHS, let's have a conversation about how private and NHS care can work together for your best outcome.
Why Patients Hesitate
The fears I hear are real:
-
"Will I offend my NHS oncologist?"
-
"Will I lose my place if I go private for one part of my care?"
-
"Can I ever go back to the NHS?"
These concerns are understandable but largely unfounded. Good private practice complements the NHS rather than competing with it.
How Coordination with the NHS Actually Works
Dr James Wilson regularly coordinate with NHS colleagues. We talk. We share information. We ensure your care is seamless, not duplicated.
Sometimes private treatment means accessing therapies that aren't widely commissioned on the NHS - like stereotactic radiotherapy for oligoprogressive disease. This isn't about "jumping ship." It's about using all available options and making them work together.
You can move between NHS and private care as needed. Many of my patients receive systemic therapies through the NHS while having SABR privately, or vice versa. The key is coordination, and that's something we prioritise for every patient.
Why Speed Matters in Cancer Treatment
Here's a practical example: Before starting SABR for oligometastatic disease, you need a PET scan to confirm there are only limited metastatic sites. On the NHS, getting that PET scan scheduled, then reviewed and reported, then starting treatment planning can take weeks.
In private practice, this all typically happens within a week.
Why does speed matter? Because cancer is active. While you're waiting, cancer can grow at existing sites or spread to new ones. The window of opportunity for treatments like SABR can close if delays allow the disease to progress.
This isn't criticism of the NHS - it's simply a reality of resource constraints versus the urgency metastatic cancer demands.
Your NHS Team Understands
NHS doctors are aware that some treatments are more readily available privately. They understand that patients sometimes need to move quickly. In my experience, most NHS oncologists appreciate when their patients can access complementary private care - it often makes their job easier because you return with better disease control.
Going private for specific treatments doesn't mean you're ungrateful for NHS care or that you've abandoned your NHS team. It means you're taking control where you can, when timing matters most.
A Coordinated Approach to Your Cancer Care
My approach is collaborative:
-
I review your NHS treatment history and coordinate with your NHS oncologist
-
If you're having systemic therapy through the NHS, I ensure SABR timing complements this
-
I provide reports to your NHS team so everyone is working from the same information
-
You maintain your NHS relationships while accessing treatments that might not be available there
Private cancer treatment doesn't replace NHS care, it complements it. All records and information shared with your NHS team if requested. Whether you're a private patient for all care or using both NHS and private services, we ensure seamless coordination.
Comprehensive, expert cancer treatment offered by Dr Wilson


-
Targeted Therapy
Proton Beam Therapy for Lung Cancer
Proton beam therapy (PBT) is a specialised & highly effective radiotherapy that targets lung tumors more accurately, reducing radiation to essential organs and tissues.
Learn more ↗ -
Targeted Therapy
Stereotactic Radiotherapy
Stereotactic radiotherapy (SABR) is a precise, high-dose radiation therapy for early-stage lung cancer. It’s highly effective, and my personal cure rate is 90%.
Learn more ↗ -
Targeted Therapy
Breakthrough Drug Therapies
Learn more ↗ -
Targeted Therapy
Chemotherapy and Immunotherapy
Chemotherapy kills rapidly dividing cancerous cells, and immunotherapy boosts the immune system’s ability to recognise and attack cancer cells.
Learn more ↗ -
Targeted Therapy
CyberKnife
CyberKnife is an advanced form of radiation therapy specifically designed to target and treat cancer with unparalleled precision. Using state-of-the-art robotics and real-time imaging.
Learn more ↗ -
Targeted Therapy
MR Linac
MR Linac is a form of stereotactic ablative radiotherapy (SABR) treatment which integrates magnetic resonance imaging (MRI) with a linear accelerator (Linac).
Learn more ↗ -
Targeted Therapy
Cancer Blood Tests: Monitoring, Treatment Planning & Early Detection
Learn more ↗

Your Private Cancer Consultant: Someone Who Understands What You're Going Through
I know what it's like when cancer comes into your family. I've sat where you're sitting - watching someone I love navigate the fear, the waiting, the maze of appointments. That experience changed how I practice medicine. It made me realise that clinical expertise matters, but so does being treated like a human being during the hardest time of your life.
About Dr James Wilson: London Oncologist & Cancer Specialist
I'm Dr James Wilson, and I've spent my career becoming the kind of oncologist I wish my family had access to: someone who answers your calls, explains things clearly, moves fast when cancer demands it, and never makes you feel like just another appointment slot.
My background: I trained at the University of Oxford, the Royal Marsden and Massachusetts General Hospital, and worked as a consultant at UCLH. I left the NHS to practice privately because I was tired of watching good people wait for treatments that should start in days.
What sets me apart professionally: I'm a Clinical Oncologist - qualified in both medical oncology (drug treatments) and radiation oncology (radiotherapy). This means you get the full range of options - SABR, proton therapy, immunotherapy, targeted drugs - coordinated by one person who knows you, your family, and your case inside out. No handoffs. No repeating your story to strangers.
I specialise in treating:
-
Lung cancer at every stage (non-small cell and small cell)
-
Melanoma and skin cancer
-
Oligometastatic disease - when cancer has spread to just a few sites
-
Complex cases requiring proton beam therapy
-
Patients who've been told "there are no more options"
The period between diagnosis and starting treatment is agonising. Let's make it as short as possible. Let's get you answers, get you a plan, and get you the treatment you need.
The benefits of private cancer care at a private oncology clinic
My practice is structured to provide comprehensive oncological care with a focus on clinical excellence and personalised attention.
Book nowPriority scheduling for urgent clinical needs (same or next day appointments)
Comprehensive treatment planning including chemotherapy, immunotherapy, and state-of-the-art radiotherapy
Direct consultant communication throughout your care
Flexible arrangements to accommodate complex cases
Access to the latest targeted therapies and stereotactic radiotherapy technologies
Rapid access to modern cancer treatments
Dr James Wilson offers personalised cancer care combining the latest systemic therapies with advanced radiotherapy techniques. Treatment plans are individually tailored using molecular profiling and latest evidence, ensuring patients receive optimal therapy for their specific cancer type and genetic profile.
Book nowImmunotherapy and checkpoint inhibitors
Targeted molecular therapies
Precision chemotherapy regimens
Stereotactic radiotherapy (SABR/SBRT including MR-linac)
Proton beam therapy for lung cancer
You Won't Leave Your Consultation Without Answers and a Clear Next Step
Cancer creates uncertainty and urgency. My promise is simple: when you meet with me, you'll walk away with clear answers about your diagnosis, a thorough explanation of all your treatment options, and a specific plan of action.
No waiting for test results. No unanswered questions. No delays in starting treatment. Just expert, compassionate care delivered at the pace your cancer demands.
Whether you're newly diagnosed, seeking a second opinion, or frustrated with delays in the NHS, let's talk. Same or next-day appointments available.
I'll get to know you and your loved ones - together we make a team with the aim of getting the best cancer treatment results for you.
Book your consultation now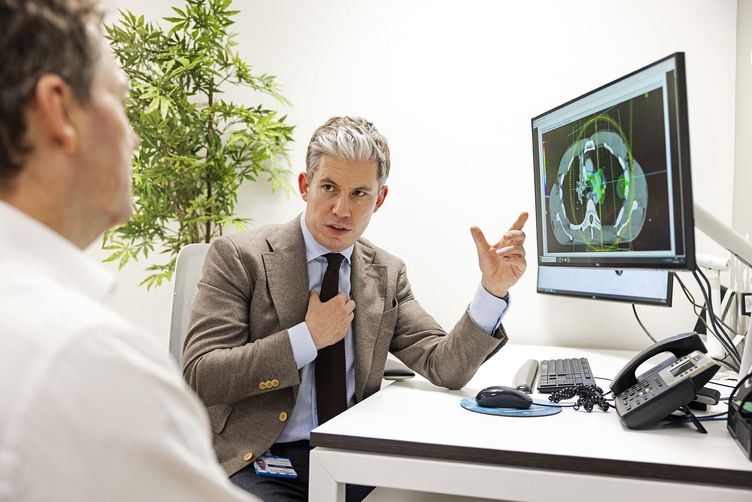
You're Not Just a Patient - You're a Person We're Here to Support
Cancer affects everyone who loves you, not just you. That's why effective cancer treatment requires more than technology and clinical care - it requires people who genuinely care.
What you can expect:
-
Dedicated oncology nurses who know you by name, providing continuous support and advice
-
Rapid access to scans and diagnostic tests—no limbo, no endless waiting
-
Clear information about treatment options, side effects, and what to expect (in plain English)
-
Clinical trials access when appropriate for your cancer type
-
Coordination with care providers, ensuring your individual needs are met
-
Support for international patients navigating care in the UK
-
Transparent guidance on private health insurance coverage and self-pay options
One of the things I love most about this work is getting to know people. We understand that people need more than medical expertise. You need support, clear information, and care that respects your life outside of treatment.
We work alongside organisations like Macmillan Cancer Support to ensure you have access to the services and information you need, with support available at every stage.
Whether you're a private patient or coordinating with the NHS, our standard is excellence in every aspect of your cancer treatment journey. More importantly, we're here when you need us.
Get in touch to learn about the wide range of ways we can support you and your family.




